When COPD and Heart Failure Overlap: What Patients Need to Know

COPD and heart failure often exist together, and when they do, symptoms can worsen quickly and become harder to untangle. Shortness of breath, fatigue, swelling, and rapid heart rate may come from the lungs, the heart, or both at the same time. In people with long-standing or advanced COPD, low oxygen levels can place constant strain on the heart, sometimes leading to a condition called cor pulmonale, a form of right-sided heart failure caused by lung disease.
In this article we’ll explain how COPD and heart failure are connected, what tests doctors use, and what practical steps patients and caregivers can take to stay safer and get the right care.
How COPD and Heart Failure Are Connected
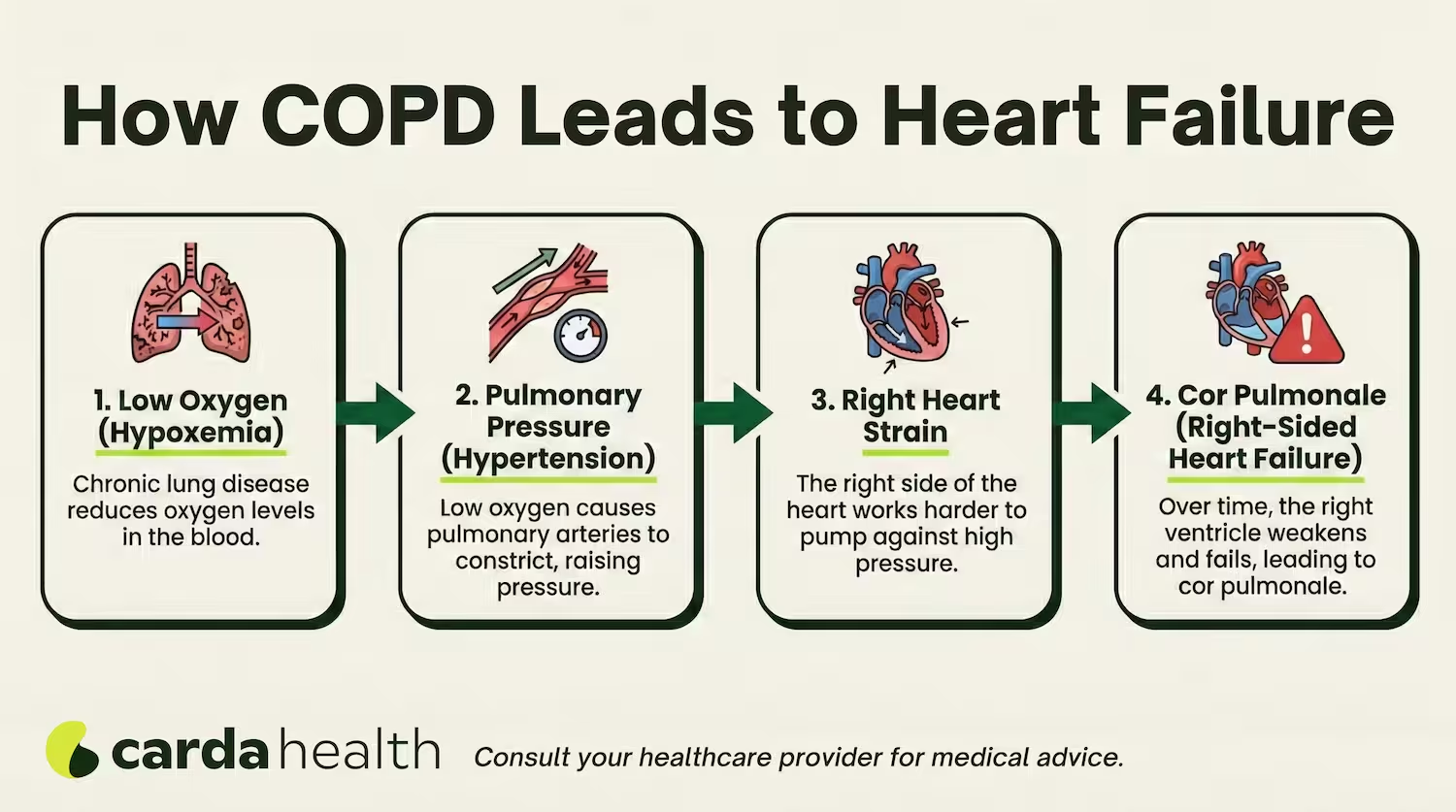
COPD doesn’t just affect the lungs. Over time, it can place significant stress on the heart, especially, when oxygen levels stay low for long periods. This ongoing lack of oxygen (called chronic hypoxia) forces the heart to work harder to pump blood through the lungs.
As COPD progresses, the blood vessels inside the lungs can become narrowed and stiff. This raises pressure in the pulmonary arteries, a condition known as pulmonary hypertension. When the right side of the heart has to pump against this higher pressure day after day, it can gradually weaken and enlarge.
Also Read: How To Reverse Pulmonary Hypertension Naturally
This process can lead to cor pulmonale, which is a specific type of right-sided heart failure caused by chronic lung disease, most commonly COPD. Unlike left-sided heart failure (often related to heart attacks or high blood pressure), cor pulmonale starts in the lungs and secondarily damages the heart.
Not everyone with COPD develops heart failure, but the risk increases with:
- Long-standing disease
- Frequent flare-ups
- Persistently low oxygen levels
- Advanced stages of COPD
This close heart–lung relationship is why people with COPD may notice new symptoms over time, such as leg swelling, faster heart rate, or worsening fatigue, even if their breathing symptoms haven’t dramatically changed.
Can COPD Cause Heart Failure?
Short answer: Yes.
COPD can contribute to heart failure, but it doesn’t happen overnight, it takes time and happens in more advanced stages.
COPD can also worsen existing heart disease. Low oxygen levels, chronic inflammation, and repeated flare-ups increase stress on the entire cardiovascular system. This is why people with COPD have a higher risk of developing congestive heart failure (CHF), particularly as they age or if other risk factors are present.
COPD vs Heart Failure: Symptoms
When COPD and heart failure happen at the same time, symptoms often feel more intense and harder to manage. Shortness of breath may occur with minimal activity or even at rest, and recovery after exertion can take longer than usual.
Patients may notice swelling in the legs or ankles, rapid or irregular heartbeats, increasing fatigue, or sudden weight gain from fluid retention. And these signs are more suggestive of heart failure. At the same time, COPD-related symptoms such as chronic cough, wheezing, chest tightness, and mucus production may continue or worsen.
Because these symptoms overlap, flare-ups can be confusing. What feels like a COPD exacerbation may actually be heart failure worsening, or both happening together. This is why tracking changes, such as swelling, weight, oxygen levels, and rescue inhaler use, is especially important when both conditions are present.
Symptoms: COPD vs Heart Failure (HF)
How Doctors Diagnose COPD vs Heart Failure
COPD and heart failure can look very similar at first. Both cause shortness of breath, fatigue, and reduced exercise tolerance. Because of this overlap, it’s common for symptoms to be mistaken for one condition when the other is also present.
Doctors start by looking at how symptoms behave. Breathlessness from COPD is usually long-standing and worsens with activity, while heart failure often causes shortness of breath when lying flat or waking suddenly at night. Swelling in the legs, rapid weight gain from fluid, and a sense of chest pressure point more toward heart failure.
Testing helps clarify the cause. Spirometry assesses lung airflow and confirms COPD, while blood tests such as BNP or NT-proBNP can suggest heart failure. Imaging tests, including chest X-rays and echocardiograms, show heart size, pumping function, and fluid buildup.
In many people, both conditions are present. When that happens, treatment focuses on identifying which problem is driving symptoms at a given time and adjusting care accordingly.
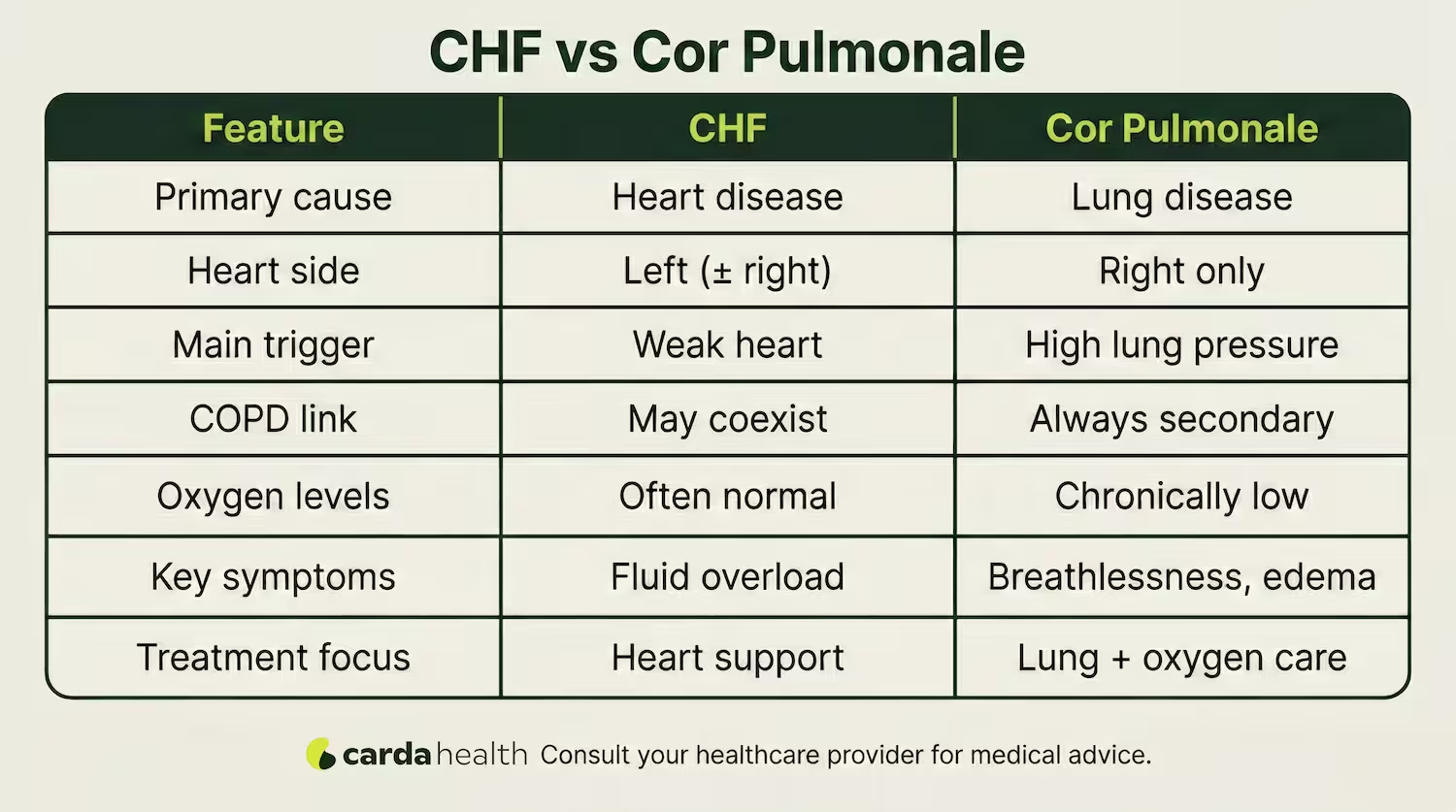
CHF vs Cor Pulmonale
Congestive heart failure (CHF) is a broad term that describes the heart’s inability to pump blood effectively to meet the body’s needs. It most commonly involves the left side of the heart and is usually caused by conditions such as coronary artery disease, high blood pressure, or prior heart attacks.
In contrast, cor pulmonale is a specific type of right-sided heart failure that develops as a direct result of lung disease, most often long-standing COPD.
While CHF can occur independently of lung disease, cor pulmonale is always secondary to a pulmonary cause. Some people with COPD may have both conditions at the same time, which makes diagnosis and treatment more complex and requires careful coordination of heart and lung care.
COPD, Heart Rate, and Blood Pressure Changes
COPD can affect how the heart beats and how blood pressure behaves. When oxygen levels are low, the body responds by increasing heart rate to deliver more oxygen to tissues. This is why many people with COPD notice a persistently higher resting heart rate, especially during flare-ups or physical activity.
A “normal” resting heart rate for adults is usually 60–100 beats per minute, but people with COPD may run closer to the upper end of that range. A sudden, sustained increase in heart rate, especially when combined with swelling or breathlessness, can signal heart failure or worsening lung disease.
Blood pressure patterns can also change. Some people develop low blood pressure from heart failure medications or dehydration, while others may have high blood pressure due to long-standing vascular strain. Monitoring trends, rather than single readings, helps doctors decide whether symptoms are coming from the heart, the lungs, or both.
Also Read: How to Increase Oxygen Levels
Treatment When You Have Both COPD and Heart Failure
Treating COPD and heart failure together requires balance. Medications that help one condition can sometimes worsen the other if not chosen carefully, so doctors usually take a coordinated approach.
For COPD, long-acting bronchodilators are commonly used to ease airflow and reduce breathlessness. In people with heart failure, doctors often prefer cardio-selective beta-blockers, which protect the heart without significantly affecting lung function. Diuretics may be added to reduce fluid buildup, easing leg swelling and lung congestion.
Oxygen therapy can help when blood oxygen levels are low, but it’s prescribed cautiously to avoid carbon dioxide retention. Pulmonary rehabilitation and gentle, supervised exercise are often recommended because they improve both breathing efficiency and heart strength. Smoking cessation, infection prevention, and careful medication review are essential to keep both conditions stable.
When to Seek Emergency Care
Some symptoms mean you need urgent medical attention, especially when COPD and heart failure coexist. Don’t wait or try to manage these at home.
Seek emergency care if you experience:
- Severe shortness of breath at rest or difficulty speaking full sentences
- Chest pain, pressure, or tightness that doesn’t improve
- Blue or gray lips or fingertips
- Confusion, extreme drowsiness, or fainting
- Rapid weight gain with worsening swelling in the legs or abdomen
- Very low oxygen levels despite using prescribed oxygen
Prompt treatment can be lifesaving and may prevent long-term complications affecting both the heart and lungs.
Life Expectancy and Outlook With COPD and Heart Failure
When COPD and heart failure occur together, the overall outlook depends on severity, stability, and how well both conditions are managed. People with mild or moderate disease who avoid flare-ups, use medications correctly, and stay active often live many years with a reasonable quality of life.
More advanced disease, especially stage 4 COPD combined with heart failure or cor pulmonale, is linked to higher hospitalization risk and shorter life expectancy. Studies consistently show that frequent exacerbations, low oxygen levels, fluid overload, and poor physical conditioning worsen outcomes.
That said, the prognosis is not fixed. Patients who stop smoking, follow treatment plans, maintain nutrition, and engage in pulmonary or cardiac rehab often do better than predicted averages. Doctors usually focus less on exact timelines and more on stability, symptom control, and preventing complications.
Conclusion
COPD and heart failure often go hand in hand, and together they can make symptoms harder to understand and manage. Knowing how these conditions interact, including the role of cor pulmonale, heart rate changes, and overlapping symptoms, helps you recognize problems early and seek the right care.
With coordinated treatment, correct inhaler use, heart-safe medications, rehabilitation, and close monitoring, many people live meaningful, active lives despite having both conditions. If symptoms change or feel harder to control, early support can make a real difference.
Carda Health’s virtual pulmonary rehabilitation program offers guided support to help you manage breathing, activity, and daily symptoms safely at home, tailored to your unique heart and lung needs.
{{book-your}}
FAQs
Can COPD lead to heart failure?
Yes. Long-term COPD can strain the heart, especially when oxygen levels stay low. Over time, this may lead to heart failure, most commonly right-sided heart failure (cor pulmonale), and can also worsen existing congestive heart failure.
What’s the difference between COPD-related heart failure and regular CHF?
COPD-related heart failure usually affects the right side of the heart and is caused by lung disease (cor pulmonale). Typical CHF more often involves the left side of the heart and is caused by heart conditions like high blood pressure or coronary artery disease.
How can I tell if my shortness of breath is from COPD or heart failure?
COPD breathlessness is usually long-standing and linked to airflow limitation, while heart failure often causes breathlessness when lying flat, leg swelling, or rapid weight gain from fluid. Doctors use lung tests, blood work, and heart imaging to tell the difference.
Does having both COPD and heart failure shorten life expectancy?
Having both conditions can increase health risks, especially in advanced disease. However, many people live for years when symptoms are controlled, flare-ups are prevented, and both heart and lung conditions are treated together.
What is cor pulmonale and why is it common in COPD?
Cor pulmonale is right-sided heart failure caused by lung disease. In COPD, chronic low oxygen raises pressure in the lung arteries, forcing the right side of the heart to work harder until it weakens.
What treatments help when COPD and heart failure occur together?
Treatment often includes inhalers, heart-safe medications, diuretics, oxygen therapy (when needed), and pulmonary or cardiac rehabilitation. Care is usually coordinated between pulmonology and cardiology to avoid medication conflicts.
References
GOLD Report 2025 – COPD comorbidities
Cor Pulmonale (Right-Sided Heart Failure)
https://www.heart.org/en/health-topics/heart-failure
Heart failure - Symptoms & causes
https://pubmed.ncbi.nlm.nih.gov/32709319/
https://publications.ersnet.org/content/breathe/21/1/240099
https://www.sciencedirect.com/science/article/pii/S014795632400061X
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063

.avif)



.avif)


