When to Get Oxygen Therapy for COPD: Who Needs It, How It Helps & How to Use It Safely
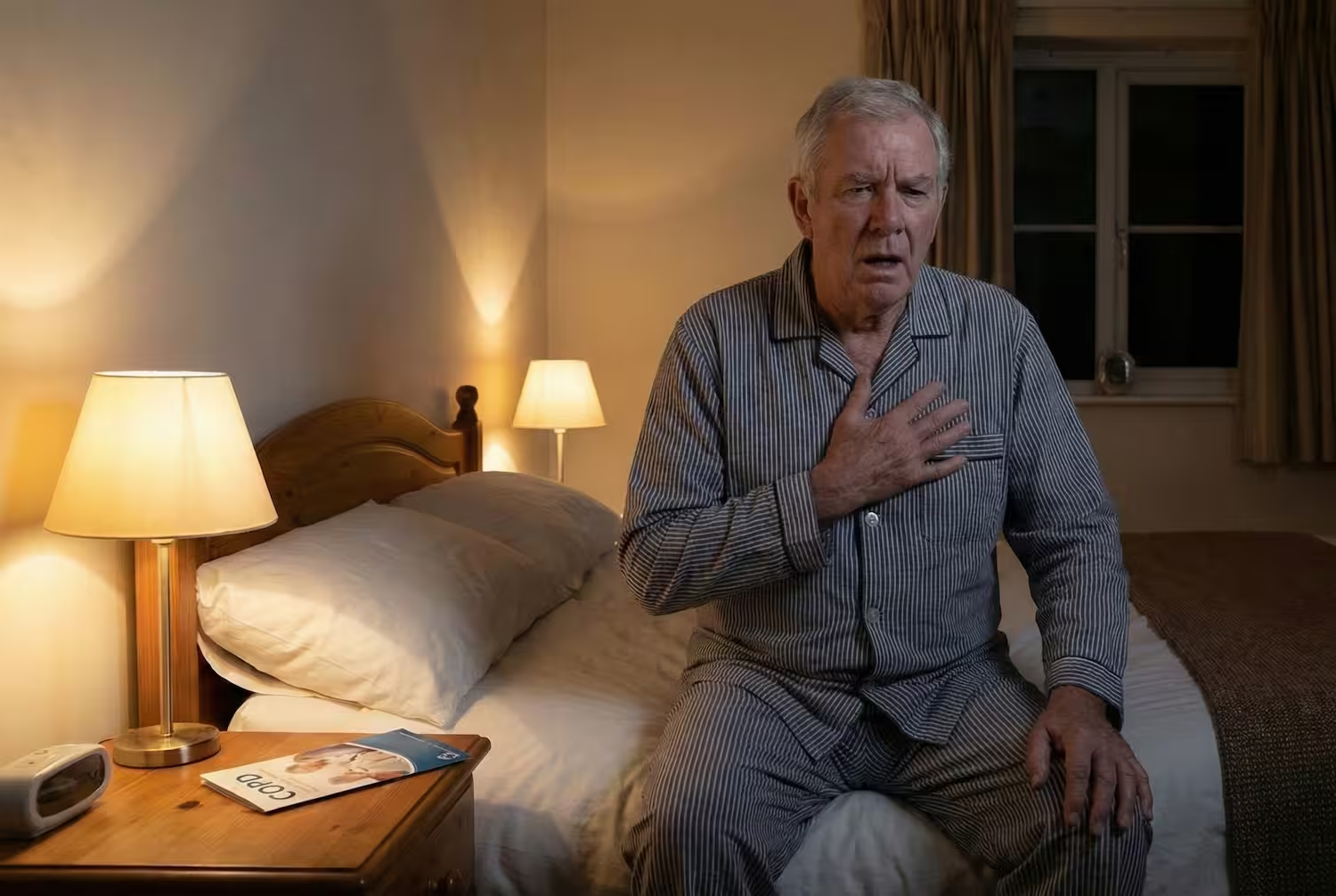
Breathlessness can become one of the hardest parts of living with Chronic Obstructive Pulmonary Disease. As the disease progresses, many people begin noticing that simple tasks like walking, talking, or even waking up in the morning feel harder than before. These changes often signal low oxygen levels, a major turning point in COPD.

Studies suggest that among patients with moderate to very severe disease, somewhere around 5% to 10% are eventually prescribed long-term oxygen therapy, and clinical trials such as the landmark NOTT/MRC studies confirm that oxygen therapy is the only treatment proven to extend life in those with severe resting hypoxemia.
That’s the reason why understanding oxygen therapy for COPD matters so much.
What Is Oxygen Therapy?
Oxygen therapy is a treatment that provides extra oxygen to people whose lungs can’t maintain safe levels on their own. For many people with COPD, especially in the moderate to very severe stages, the lungs become too damaged to move enough oxygen into the bloodstream.
Oxygen therapy raises your oxygen saturation back into a safer range, reduces symptoms, improves sleep, and can even extend life in certain cases. When used correctly, oxygen becomes one of the most effective long-term treatments for advanced COPD.
Common oxygen options include:
- Home oxygen concentrators
- Portable oxygen concentrators (POCs)
- Compressed oxygen tanks
- Liquid oxygen systems
Your doctor decides the ideal device and flow rate based on your symptoms and oxygen test results.
Oxygen therapy for COPD Guidelines & LTOT Criteria
Doctors prescribe long-term oxygen therapy when oxygen levels fall below a medically safe range. According to the GOLD 2025 guidelines and American Thoracic Society (ATS) recommendations, oxygen therapy is typically recommended when:
SpO₂ ≤ 88% at rest, or
PaO₂ ≤ 55 mm Hg, confirmed by arterial blood gas testing
PaO₂ 56–59 mm Hg with complications such as:
- Cor pulmonale
- Polycythemia
- Peripheral edema
Some people have normal oxygen levels while resting but drop below 88% only during walking or exercise. In this case, doctors may prescribe ambulatory oxygen for use during activity.
Nighttime oxygen may also be needed if oxygen levels fall during sleep.
These decisions are based on objective testing, no one should change flow rates or start oxygen without medical guidance.
Does Oxygen Therapy Actually Help?
Studies show that oxygen therapy (OT) has been proven to extend life in patients with severe resting hypoxemia. This benefit applies only to people with very low oxygen levels at rest (≤ 88%).
Many patients who start oxygen therapy often report improvements such as; less breathlessness, better sleep quality, fewer morning headaches, improved mental clarity, & more energy for daily activities.
It is important to know that OT does not reverse lung damage but protects vital organs from low oxygen.
Types of Oxygen Therapy for COPD
Not everyone with COPD needs the same type of oxygen system. Doctors choose the device based on how low your oxygen levels are, how active you are, and whether you need support only during activity or all day long.
Here are the most common options patients use:
1. Oxygen Concentrators (Home Units)
Provide continuous oxygen pulling from air, using electricity. Reliable and cost-effective.
2. Portable Oxygen Concentrators (POCs)
Battery-powered, lightweight, and FAA-approved for flights.
3. Compressed Oxygen Tanks
Do not require electricity; commonly used for short trips or backup.
4. Liquid Oxygen Systems
High-capacity, lighter tanks for patients needing higher flow rates. Availability varies.
5. COPD Oxygen Mask
While nasal cannulas are used most often because they’re more comfortable for long-term therapy, Oxygen masks may be used in specific situations such as higher flow needs, during flare-ups, or when a person cannot tolerate the cannula.
Tips to Use Oxygen Safely at Home
Oxygen therapy is safe when used correctly, but it does require some awareness and simple precautions. These steps help you stay comfortable, avoid complications, and prevent accidents.
1. Keep oxygen away from flames or heat
2. Use the flow rate exactly as prescribed
3. Prevent tubing accidents & long tubing
4. Have a backup plan for power outages
5. Use a fan or cool air for breathlessness.
Living With Oxygen: Moving, Sleeping, Traveling & Daily Life Tips
Walking & Light Exercise
Using ambulatory oxygen helps you stay active safely. Make sure to use a portable concentrator or small tank with wheels. Keep the tubing short enough to move easily.
Sleeping With Oxygen
Sleeping may be one of the most important times to use oxygen. It prevents nighttime dips, morning headaches, and breathlessness.
Air Travel With Oxygen
You can fly with COPD, but it requires planning. Most airlines allow FAA-approved portable oxygen concentrators (POCs). To prepare:
- Talk to your doctor at least 2 weeks before travel
- Get medical clearance from the airline
- Carry extra batteries (usually 1.5x the flight duration)
- Bring your prescription and oxygen settings
High altitude can lower oxygen levels, so flying without a POC is not recommended for most COPD patients.
Driving
Yes, you can drive while using oxygen if you feel alert and stable. Secure the device and avoid smoking in the car, and you are good to go.
Showering, Cooking & Daily Tasks with Oxygen
Sit on a shower chair to avoid shortness of breath. Avoid cooking over open flames while wearing oxygen. Use a crossbody bag or backpack to carry portable units around the house, and if you feel tired, break tasks into short steps
Some people feel self-conscious when they first start oxygen therapy. This initial discomfort is normal, but most patients feel better once their symptoms improve.
Costs & Insurance of Oxygen Therapy
Since every patient’s needs are different, costs can vary. But most people pay far less than they expect once coverage and home-delivery services are in place.
Oxygen therapy requires a prescription, which your doctor writes after confirming low oxygen levels through pulse oximetry or an arterial blood gas test. The prescription includes your flow rate, when you should use oxygen (rest, sleep, activity, or full-time), and the type of device you need. Once it’s issued, a home-oxygen supplier will set up your equipment, teach you how to use it, and arrange ongoing support.
Most insurance plans, including Medicare, and many private insurers, cover oxygen therapy if medical criteria are met, such as SpO₂ of 88% or lower at rest or PaO₂ of 55 mm Hg or below. Coverage usually includes a home concentrator, tubing, cannulas, a portable system, and regular maintenance or refills.
Out-of-pocket costs vary, but with insurance, patients typically pay only a small monthly copay, while without coverage equipment rentals can cost anywhere from $70 to $200 per month depending on the device.
Common Myths & Misconceptions
Myth 1: “If I start using oxygen, I’ll become dependent on it.”
Truth: You do not become “dependent” on oxygen in the sense of addiction. If your oxygen levels are low, your body already needs oxygen — the extra oxygen simply keeps your organs safe. Using oxygen doesn’t weaken your lungs; it supports them.
Myth 2: “Oxygen will make my lungs lazy.”
Truth: Oxygen does not weaken lung muscles. It prevents your heart and brain from being damaged by low oxygen levels. Breathlessness often comes from airflow obstruction, not lack of oxygen.
Myth 3: “More oxygen is better.”
Truth: Higher flow rates can be dangerous for people who retain carbon dioxide. Your doctor prescribes a specific flow rate to keep your SpO₂ in a safe range (usually 88–92%).
You should never change your oxygen level without medical guidance.
Myth 4: “Using oxygen means my COPD is at the end stage.”
Truth: Many people start oxygen therapy in moderate or severe COPD, especially when oxygen dips during walking or sleep. Oxygen doesn’t define your stage, it’s simply a tool to help you feel better and stay safer.
Myth 5: “I won’t be able to leave the house anymore.”
Truth: Portable oxygen concentrators and lightweight tanks are designed specifically to help people stay mobile.
Myth 6: “Oxygen is only for people who are dying.”
Truth: Oxygen therapy is a long-term treatment, not an end-of-life measure. People use it for years to protect their heart, improve stamina, and prevent complications from low oxygen.
Myth 7: “It’s embarrassing to wear oxygen in public.”
Truth: Millions of people use oxygen worldwide, and portable devices are smaller and more discreet than ever.
Myth 8: “Oxygen cures COPD.”
Truth: Oxygen doesn’t repair lung damage, no treatment can reverse COPD. Still it improves your chances of living slightly better as long as possible, and it is one of the most effective supportive treatments available.
Conclusion
Oxygen therapy may feel like a big adjustment, but it can make life with COPD safer, more comfortable, and more manageable. It protects your heart and brain, reduces breathlessness, and may extend life in people with severely low oxygen levels. With the right setup, support, and medical guidance, OT becomes a reliable partner in your day-to-day routine.
If you’re feeling unsure about whether oxygen is right for you, talk openly with your doctor.
Carda Health supports patients at every stage, helping you stay active, breathe easier, and manage COPD with confidence and clarity.
FAQs
Does oxygen help breathlessness?
Yes, if your oxygen levels are low. Oxygen improves stamina, reduces breathlessness during activity, and can improve sleep and mental clarity. But if your oxygen level is normal, oxygen will not fix shortness of breath caused by airflow obstruction.
Can oxygen extend life?
Long-term oxygen therapy (LTOT) improves survival in people with severe resting hypoxemia (very low oxygen levels at rest). This is one of the most proven benefits of oxygen therapy.
Can you use too much oxygen?
Using more oxygen than prescribed may increase carbon dioxide levels in some COPD patients. Always stick to your doctor’s flow rate unless told otherwise.
Do I need oxygen forever?
Not always; some use it only during sleep or activity. Others, especially in later stages, need it long-term.
Is it safe to sleep with oxygen?
Yes, and for many people, nighttime is when oxygen is most helpful.
Can you shower with oxygen?
Yes, with precautions. Keep a portable tank placed outside the shower, & use a longer tubing length.
Can you fly with oxygen?
Yes, using an FAA-approved portable concentrator.
References
GOLD – Global Initiative for Chronic Obstructive Lung Disease (2025 Report)
Home Oxygen Therapy for Adults with COPD: An Official ATS Clinical Practice Guideline
NHLBI - COPD Treatment and Oxygen Therapy
Oxygen for Relief of Breathlessness in Patients with Chronic Obstructive Pulmonary Disease
Long-term oxygen treatment in COPD: Recommendations and review of evidence





.avif)


