How COPD Affects Your Sleep — And What You Can Do About It
COPD and Sleep: Overlap Syndrome, CPAP, Tests & Sleep Tips
COPD and sleep problems often go hand in hand. Studies show that 53% of people with COPD report poor sleep quality, including difficulty falling asleep, frequent nighttime awakenings, and waking up short of breath. Nighttime oxygen levels can drop significantly in COPD, especially during REM sleep, which places extra strain on the lungs and heart.
In some patients, COPD also overlaps with obstructive sleep apnea (OSA), a combination known as overlap syndrome, which is linked to higher risks of flare-ups, hospitalizations, and cardiovascular complications if left untreated. Because sleep plays a critical role in breathing control, energy levels, and overall health, addressing sleep issues is an essential part of COPD care, not just a comfort issue.
Why Do People With COPD Have Sleep Problems?
Several changes that happen in COPD make sleep more difficult. At night, breathing naturally slows and becomes shallower. In people with COPD, this can lead to lower oxygen levels and higher carbon dioxide levels, especially during REM sleep. These nighttime changes often trigger awakenings, breathlessness, or a feeling of air hunger.
Symptoms that wake you
Symptoms also play a role. Chronic cough, mucus buildup, wheezing, and chest tightness can interrupt sleep repeatedly. Lying flat may worsen shortness of breath for some people, while anxiety related to breathing can make it harder to fall asleep in the first place.
Medications and other reasons
Medications and lifestyle factors matter too. Some inhalers can cause mild stimulation if taken too close to bedtime, and smoking or caffeine use in the evening further disrupts sleep. Over time, poor sleep leads to daytime fatigue, reduced activity, and lower quality of life, which can worsen COPD symptoms overall.
Also Read: How to manage COPD at home
Is COPD worse at night or morning?
COPD symptoms are often worse at night and early morning. At night, lying flat and slower breathing can worsen oxygen levels. In the morning, mucus buildup and airway stiffness after sleep can make breathing feel harder until medications and movement help open the lungs.
COPD-OSA Overlap (Overlap Syndrome)
Some people with COPD also have obstructive sleep apnea (OSA). When both conditions occur together, it’s known as overlap syndrome. During sleep, repeated airway collapse from OSA combines with COPD-related airflow limitation, leading to deeper and longer drops in oxygen levels than either condition alone.
Overlap syndrome is linked to worse outcomes. Studies show higher rates of COPD exacerbations, hospitalizations, and cardiovascular complications compared with COPD alone. Untreated overlap places added strain on the heart and lungs during sleep.
How Treatment Improves Outcomes
Treating OSA with positive airway pressure (CPAP or BiPAP) helps stabilize nighttime breathing and oxygen levels. Evidence shows that appropriate PAP therapy in overlap syndrome is associated with fewer flare-ups, improved sleep quality, and better survival in selected patients.
Who Should Be Evaluated for Overlap Syndrome
Doctors are more likely to suspect overlap syndrome if a person with COPD also has symptoms like loud snoring, breathing pauses during sleep, excessive daytime fatigue, headaches, obesity or large neck circumference etc.
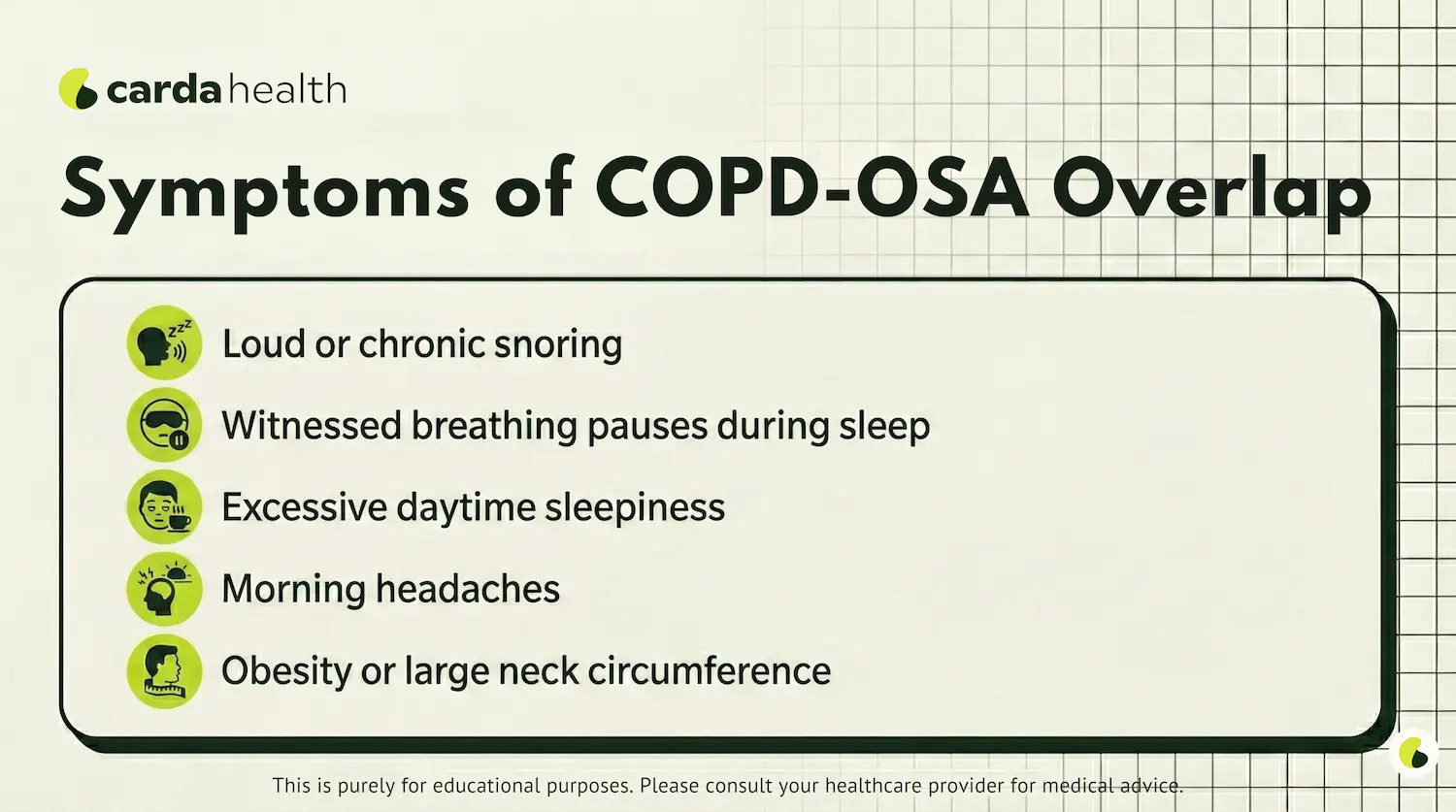
Early identification of symptoms and treatment can significantly improve both nighttime breathing and daytime function.
How Doctors Test for Sleep Problems in COPD
Doctors may recommend sleep testing if someone with COPD has worsening nighttime breathlessness, unexplained fatigue, or frequent COPD flare-ups.
Common Tests Doctors Use
Testing usually starts with a detailed sleep and symptom history, followed by targeted studies:
- Overnight pulse oximetry to check for oxygen drops during sleep
- Sleep studies (polysomnography) to diagnose obstructive sleep apnea and overlap syndrome
- Home sleep tests in selected patients with high suspicion for OSA
- Arterial blood gas (ABG) testing if nocturnal hypoventilation or high carbon dioxide levels are suspected
Sleep-related breathing problems can worsen COPD outcomes if left untreated.
Also Read: How to Test Yourself For COPD
Treatments of Sleep disorders in COPD
After identifying conditions like overlap syndrome, doctors choose the right therapy, such as CPAP, BiPAP, or nighttime oxygen, and reduce the risk of flare-ups, hospitalizations, and heart strain for the patient. Here are some of the most common treatments.
1. Positive Airway Pressure (CPAP or BiPAP)
CPAP: If overlap syndrome (COPD + OSA) is diagnosed, Continuous Positive Airway Pressure (CPAP) is often the first-line treatment doctors suggest. It is a machine, connected by a hose to a mask, that provides a continuous flow of air that creates pressure greater than atmospheric pressure, keeping the upper respiratory tract open.
It simply keeps the airway open during sleep and reduces oxygen drops.
BiPAP/NIV: It may be used when breathing effort is high or carbon dioxide levels rise at night. When used consistently, BiPAP (Bilevel Positive Airway Pressure) therapy can improve sleep quality and reduce flare-ups.
The machine pumps air through a tube to a face or nasal mask, helping to keep airways open, reduce carbon dioxide buildup, and increase oxygen levels.
Unlike CPAP, which provides a single constant pressure, BiPAP's two distinct levels make it more comfortable for patients who need higher pressure to breathe in but struggle to exhale against that same pressure.
2. Nighttime Oxygen (When Prescribed)
Some people with COPD experience nocturnal oxygen desaturation even without sleep apnea. In these cases, doctors may prescribe supplemental oxygen at night, but only after testing. Oxygen is tailored carefully to avoid carbon dioxide retention.
Also Read: When to Get Oxygen Therapy for COPD
3. Medication Timing & Symptom Control
Optimizing inhaler timing can reduce nighttime symptoms. Long-acting bronchodilators taken earlier in the evening may help prevent nocturnal breathlessness. If cough or mucus disrupts sleep, targeted treatments (airway clearance, humidification) can help.
4. Insomnia-Focused Care
Poor sleep in COPD isn’t always due to breathing alone. Cognitive Behavioral Therapy for Insomnia (CBT-I) is preferred over sleep medications and can improve sleep duration and quality without affecting breathing.
Lifestyle Adjustments To Sleep Better w/ COPD
Small changes like changing sleep position, avoiding smoking, alcohol, and heavy meals before sleep, using a cool, humidified bedroom environment, and pacing evening activity to prevent late-night breathlessness can significantly help manage sleep issues and avoid exacerbations.
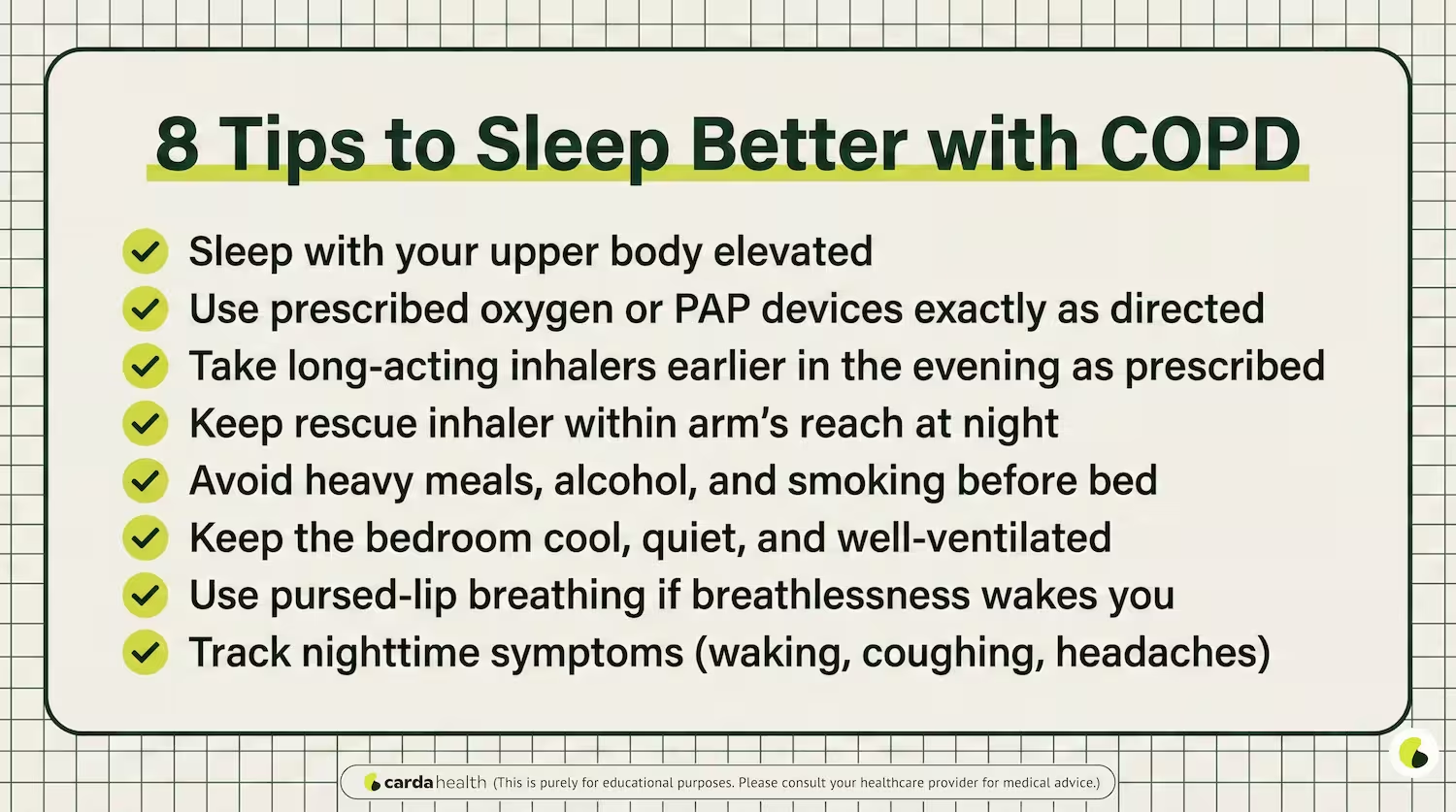
Best sleeping position with COPD
The best sleeping position for COPD patients is usually on your side or with your upper body slightly elevated. Raising your head and chest helps keep airways open, improves breathing, and reduces nighttime coughing and breathlessness. Sleeping flat can worsen symptoms, while gentle elevation often makes breathing more comfortable through the night.
When Sleep Problems Need Medical Attention
Sleep issues in COPD aren’t just uncomfortable, they can signal worsening disease or dangerous complications. Get medical help if you notice any of the following:
- Waking up short of breath or gasping
- Morning headaches, confusion, or extreme grogginess (possible CO₂ retention)
- Blue or gray lips/fingertips during the night
- Repeated nighttime awakenings with chest tightness
- Very low oxygen readings overnight (if you monitor at home)
Untreated sleep problems can raise the risk of exacerbations, heart strain, hospitalizations, and reduced quality of life. Early testing and the right therapy can improve outcomes.
Why do people with end-stage COPD sleep so much?
In advanced COPD, the body uses a great deal of energy just to breathe. Low oxygen levels, high carbon dioxide, muscle weakness, medications, and overall physical decline can cause extreme fatigue and long sleep periods. Sleeping more does not always mean the condition is worsening suddenly, but it often reflects the body conserving energy and needing more rest.
Can COPD cause death during sleep?
Death during sleep from COPD is uncommon, but it can happen in advanced stages when oxygen levels drop dangerously low or carbon dioxide builds up overnight. The risk is higher in people with severe COPD, untreated sleep apnea, respiratory failure, or heart complications. Warning signs include morning headaches, confusion, extreme fatigue, or waking up gasping for air. Using prescribed oxygen or ventilation and treating sleep apnea greatly reduces this risk.
Conclusion
Living with COPD can make nights feel long and exhausting, but poor sleep is not something you have to “just live with.” Breathlessness, oxygen drops, coughing, and anxiety at night are common, but they are also treatable when the cause is identified early. Simple steps like adjusting sleep position, timing medications better, using oxygen correctly, or addressing sleep apnea can make a real difference in how you feel day to day.
If COPD symptoms are affecting your sleep, Carda Health’s virtual pulmonary rehab and respiratory care programs can help you manage breathing, oxygen use, and nighttime symptoms from home, guided by professionals who understand COPD.
{{get-personalized}}
FAQs
Can COPD cause sleep problems?
Yes. COPD can cause breathlessness, coughing, oxygen drops, and anxiety at night, all of which disrupt normal sleep. Many people with COPD wake up frequently or feel unrefreshed in the morning.
Why is sleep worse at night with COPD?
At night, breathing naturally slows and lung mechanics change. In COPD, this can lead to lower oxygen levels, air trapping, and carbon dioxide buildup, especially during REM sleep.
What is COPD, sleep apnea overlap syndrome?
This is when a person has both COPD and obstructive sleep apnea (OSA). It increases the risk of severe nighttime oxygen drops, heart problems, and COPD exacerbations, and often requires CPAP or BiPAP therapy.
Does oxygen therapy improve sleep in COPD?
For people with low nighttime oxygen levels, prescribed oxygen can improve sleep quality and reduce strain on the heart. Oxygen should only be used at the flow rate your doctor recommends.
Can sleeping position help COPD symptoms at night?
Yes. Sleeping with the upper body slightly elevated or on your side can reduce breathlessness, coughing, and reflux, which often worsens nighttime symptoms.
When should someone with COPD get a sleep study?
A sleep study is recommended if there is loud snoring, gasping at night, severe daytime sleepiness, morning headaches, or unexplained worsening of COPD symptoms.
References
Sleep Disorders in Chronic Obstructive Pulmonary Disease: Etiology, Impact, and Management - PMC
Full article: Chronic obstructive pulmonary disease and obstructive sleep apnea overlap: who to treat and how
Overlap Syndrome (COPD and OSA): A Treatable Trait for Triple Treatment? - PMC
CPAP in overlap syndrome: Unveiling the evidence - CHEST Physician
POCKET-GUIDE-GOLD-2024-ver-1.2-11Jan2024_WMV.pdf
The use of continuous positive airway pressure in COPD-OSA overlap syndrome: A systematic review - ScienceDirect
Global prevalence of COPD–OSA overlap syndrome: A systematic review and meta–analysis - ScienceDirect
Unraveling the Complexity of COPD and Obstructive Sleep Apnea Coexiste | COPD
Factors responsible for poor sleep quality in patients with chronic obstructive pulmonary disease
REM Sleep: What It Is and Why It’s Important
Cognitive Behavioral Therapy for Insomnia (CBT-I): An Overview




.avif)

.avif)


