Inhalers for COPD: A Complete Guide to Types, Uses, and What to Expect

Inhalers are the main treatment for Chronic Obstructive Pulmonary Disease (COPD), and if you’ve been prescribed an inhaler, it’s normal to have questions like why you’re on a specific one and what it’s meant to do.
The goal of inhalers isn’t just short-term relief. They’re used to open the airways, reduce breathlessness, prevent flare-ups, and help you stay active and independent for as long as possible. Different inhalers serve different purposes, and many people need more than one over time.
In this guide, we’ll explain the main types of COPD inhalers, how doctors choose them, and how to know if your inhaler is working, using clear and practical language.
Rescue vs Maintenance Inhalers
COPD inhalers generally fall into two main categories, and knowing the difference helps you use them correctly.
Rescue Inhalers
These are fast-acting. They’re used when you feel sudden shortness of breath or chest tightness. These inhalers relax the airway muscles quickly, but their effect is short-lived. If you find yourself relying on a rescue inhaler every day, it’s often a sign that your long-term treatment needs adjustment.
Maintenance Inhalers
These are taken every day, even when you feel okay. Their job is to keep airways open over time, reduce ongoing inflammation or tightening, and lower the risk of flare-ups. They don’t work instantly, but they play the biggest role in controlling COPD day to day.
Many people with COPD use both types together, one for immediate relief, and one (or more) to keep symptoms under control long term.
4 Main Types of Inhalers Used for COPD
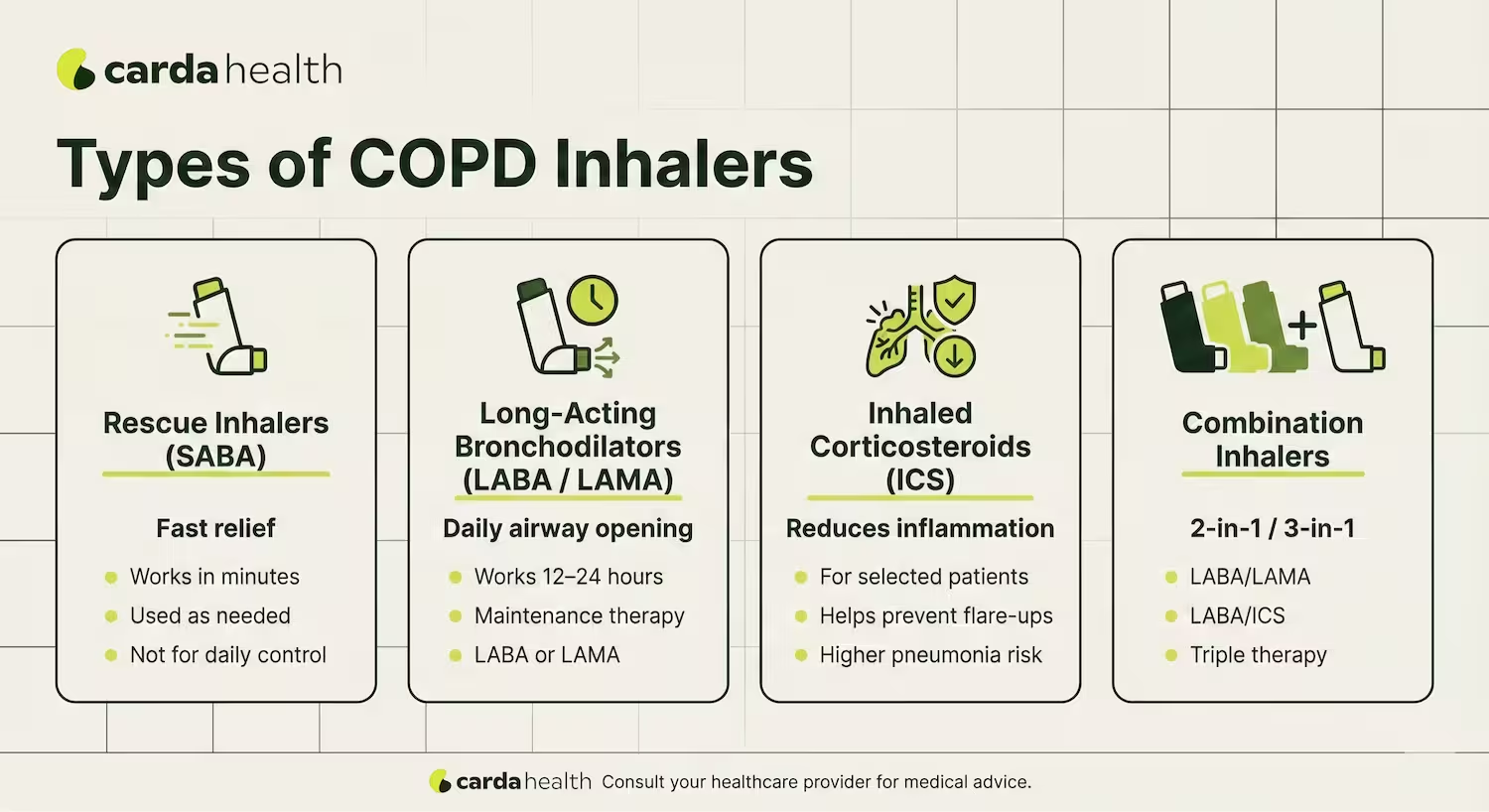
Doctors choose inhalers based on your symptoms, lung function, and history of flare-ups. Each type works in a different way, and some are often combined.
Bronchodilator inhalers
These inhalers relax the muscles around your airways so air can move more freely.
Short-acting bronchodilators:
They provide quick relief and are usually rescue inhalers.
Long-acting bronchodilators:
These are taken daily to keep airways open over many hours. Doctors further divide long-acting bronchodilators into two groups:
LABA (Long-Acting Beta-Agonists) relax airway muscles through one signaling pathway.
LAMA (Long-Acting Muscarinic Antagonists) reduce airway tightening and mucus through a different pathway.
Because they work differently, LABA and LAMA are often combined for stronger symptom control. This step-wise approach aligns with GOLD treatment recommendations.
Anticholinergic inhalers
These inhalers (often called muscarinic antagonists) reduce airway tightening and mucus production. These are commonly used as long-term control medications in COPD.
Inhaled corticosteroids (ICS)
These inhalers help reduce airway inflammation, but they’re strictly not for everyone with COPD
Doctors usually add ICS when:
- A person has frequent exacerbations
- Blood tests show higher eosinophil levels
- There is overlap with asthma features
ICS can lower flare-up risk in selected patients, but they also carry an important consideration: a higher risk of pneumonia, especially in older adults or those with severe disease.
For this reason, ICS is rarely used alone in COPD and is carefully prescribed as part of combination therapy.
Combination Inhalers
Combination inhalers simplify treatment by putting more than one medications into one device. Common types include:
LABA + LAMA
Often used when symptoms persist on a single bronchodilator.
LABA + ICS
Considered when inflammation and frequent exacerbations are present.
Triple Therapy (LABA + LAMA + ICS)
Used in more advanced COPD, or when flare-ups continue despite dual therapy.
Doctors carefully consider symptoms, exacerbation history, lung function, and infection risk before stepping up to combination or triple therapy. Your inhaler plan may change over time, and this is normal and part of good COPD care.
Inhaler Devices: MDI vs DPI vs Soft Mist vs Nebulizer
COPD medications can be delivered through different inhaler devices. The medicine inside may be similar, but how it gets into your lungs depends on the device, and that can affect how well it works for you.
COPD Inhaler Devices Comparison
Doctors usually consider symptom severity, hand strength, coordination, and daily routine when choosing the right device.
If an inhaler feels hard to use, it’s worth asking your doctor whether a different device might work better for you.
How Doctors Adjust (Step Up) Inhaler Treatment
COPD inhaler therapy is adjusted gradually, not all at once. Doctors follow a step-by-step approach recommended by the GOLD (Global Initiative for Chronic Obstructive Lung Disease) to match treatment with symptoms, flare-up risk, and safety.
Step 1: Starting With a Long-Acting Bronchodilator
Most people with COPD begin treatment with a single long-acting bronchodilator, either a LABA or a LAMA.
For many patients with mild to moderate symptoms, this level of treatment provides meaningful relief in reducing baseline breathlessness.
Step 2: Adding a Second Long-Acting Bronchodilator
If shortness of breath continues or daily activities remain limited, doctors often add a second bronchodilator (LABA + LAMA).
Using two medications that work through different pathways improves airflow more effectively than increasing the dose of just one inhaler.
Step 3: Inhaled Steroids or Triple Therapy
Inhaled corticosteroids (ICS) are added more selectively. Doctors typically consider triple therapy (LABA + LAMA + ICS) when:
- Flare-ups continue despite dual bronchodilators
- Blood eosinophil levels suggest airway inflammation
- There are asthma-like features or overlap
Because steroid inhalers can increase the risk of pneumonia in some people, this step is reviewed carefully and adjusted over time.
Why Treatment Changes Over Time
COPD is a progressive condition, and inhaler needs can change. Adjusting treatment doesn’t mean failure, it reflects ongoing optimization to balance symptom relief, flare-up prevention, and long-term safety.
When inhaler therapy alone isn’t enough, doctors may advise oxygen therapy to maintain oxygen levels of the patient.
Common vs Serious Side Effects of Inhalers
COPD inhalers are generally safe when used as prescribed, but side effects can happen. Most are mild, especially early on, and knowing what’s normal and can be managed at home, versus what needs medical advice helps you stay confident with treatment.
Common or Mild Side Effects
These often improve as your body adjusts:
- Dry mouth or throat irritation (common with bronchodilators)
- Mild shakiness or tremor
- Feeling a faster heartbeat
- Hoarseness or sore throat (more common with steroid inhalers)
Rinsing your mouth after using inhalers that contain steroids helps reduce irritation and lowers the risk of oral thrush.
Serious Side Effects That Need Medical Attention
Contact your doctor if you notice:
- Repeated chest infections or worsening cough
- Fever, chills, or thick, discolored mucus
- Sudden or unexplained worsening of breathing
- Chest tightness that doesn’t improve after rescue medication
In some people, inhalers that contain corticosteroids may increase the risk of pneumonia, especially with long-term use. This is why doctors regularly review whether these medications are still appropriate.
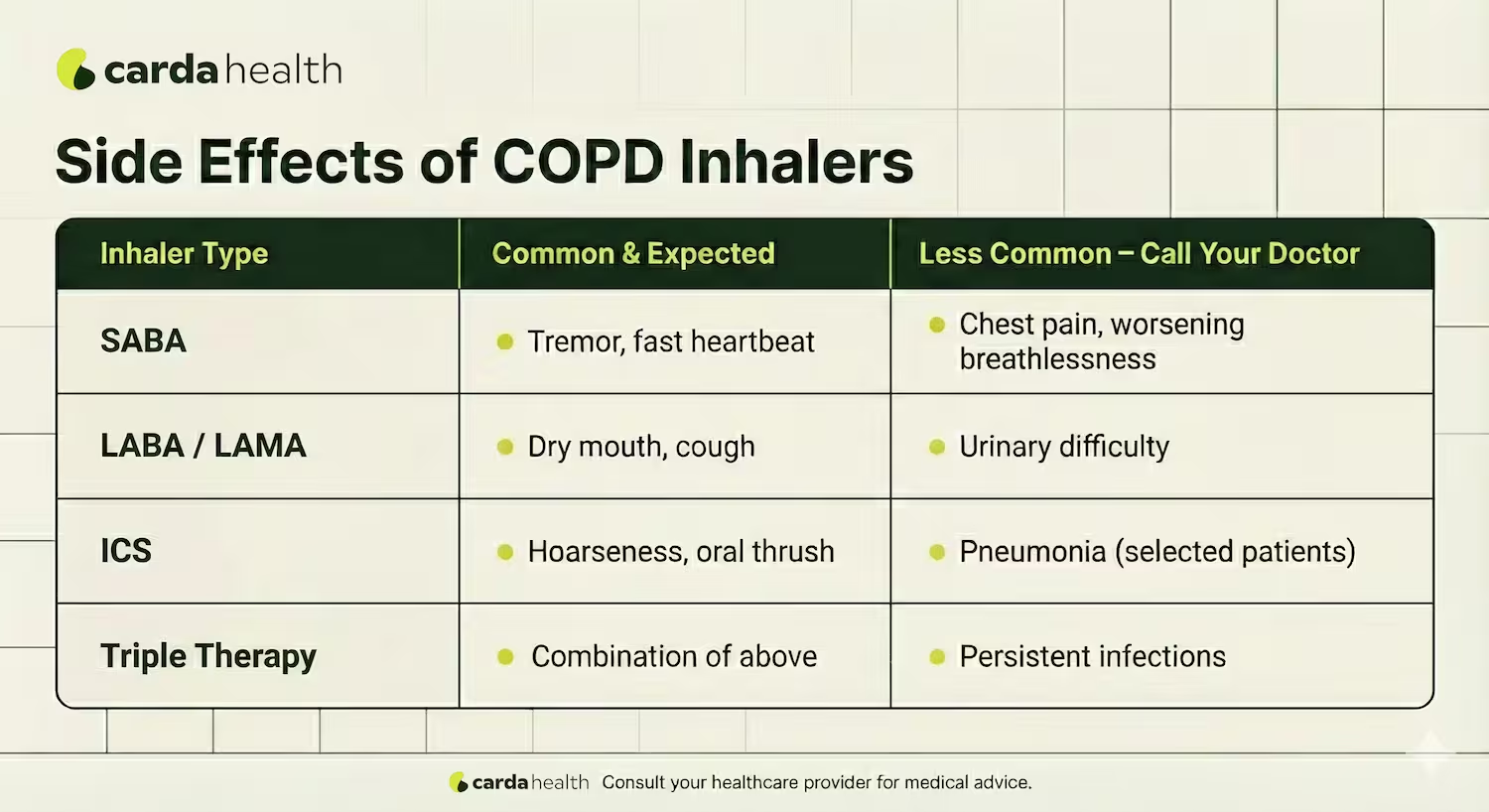
What To Do Next?
Even if side effects are a problem, DO NOT stop your inhaler on your own. Many issues can be improved by adjusting the dose, switching to a different inhaler device, or changing the medication combinations.
Your healthcare team’s goal is to balance symptom control with safety, so always speak up if something doesn’t feel right.
How to Know If Your Inhaler Is Working
It’s not always obvious whether a COPD inhaler is helping, especially because maintenance inhalers work gradually, not instantly. Instead of focusing on how you feel right after a dose, it’s more useful to look at patterns over time.
A working inhaler usually means you’re less short of breath during daily activities. You may notice that you’re reaching for your rescue inhaler less often, and that symptoms like chest tightness or wheezing are more controlled.
Another important sign is fewer flare-ups. If you’re having fewer urgent visits, infections, or courses of steroids or antibiotics, your maintenance inhaler is likely doing its job.
Also Read: How to Test Yourself For COPD At Home
What If Your Inhaler Isn’t Working?
If your symptoms haven’t improved after several weeks, or if they’re getting worse, it usually means your plan needs adjustment, a different medication, a combination inhaler, or a device that’s easier to use.
Regular check-ins with your doctor help make sure your inhaler therapy keeps working as your needs change.
Common Inhaler Mistakes (and How to Fix Them)
Many people don’t get full benefit from their inhaler because of small technique issues. These are common, and fixable mistakes.
1. Not breathing out fully before using the inhaler
Always exhale completely before each dose so the medication can reach deeper into the lungs.
2. Using the wrong breathing speed
- Metered-dose inhalers (MDIs): slow, steady inhale
- Dry powder inhalers (DPIs): fast, strong inhale
Using the wrong technique leaves medication in the mouth instead of the lungs.
3. Skipping mouth rinsing after steroid inhalers
This increases the risk of hoarseness and oral thrush. Rinse and spit after every use.
4. Poor coordination or hand strength
If pressing or inhaling at the right time is difficult, ask about spacers, soft-mist inhalers, or nebulizers.
5. Using an inhaler that feels uncomfortable or confusing
Difficulty using a device often leads to missed doses or poor delivery, switching devices can improve results without changing medication.
Fixing these small issues often improves breathing more than increasing medication doses.
Cost, Insurance & Affordability
The cost of COPD inhalers can vary widely depending on the medication, insurance coverage, and where you fill your prescription. Without insurance, brand-name maintenance inhalers often cost hundreds of dollars per inhaler, but there are ways to make treatment more affordable.
Typical Price Ranges (U.S. retail)
As of the day this article is initially published - 01/10/2026
Rescue inhalers (e.g., albuterol HFA) may cost around $100 without insurance; discount cards can sometimes lower this to ~$20–$30.
Long-acting maintenance inhalers (LABA, LAMA, or combination) commonly range from $250 to $500+ per inhaler without discounts.
Combination triple-therapy inhalers (LABA/LAMA/ICS) like Trelegy or Breztri may cost $650+ per inhaler at retail prices without insurance.
Insurance & Medicare Coverage
Most Medicare Part D plans cover both rescue and maintenance inhalers, but out-of-pocket costs vary by plan tier. Generic options may cost as little as $10–$30 per month, while brand names often carry higher copays.
Internationally, affordability studies show that inhaler costs can represent several days’ wages in some regions for comparable medications, highlighting the importance of insurance support and patient assistance where available.
Conclusion
COPD inhalers play a central role in helping you breathe easier, stay active, and reduce flare-ups. Understanding what’s inside your inhaler, how it works, and how to use it correctly can make a real difference in how well your treatment works.
If symptoms persist, side effects become bothersome, or costs are a barrier, don’t hesitate to talk with your healthcare team. Small changes, whether in medication, device, or technique, can lead to meaningful improvements in comfort and quality of life.
Carda Health combines pulmonary rehab, education, and ongoing guidance to help you breathe easier and stay active.
{{get-personalized}}
FAQs
What is the best inhaler for COPD?
There isn’t one “best” inhaler for everyone. The right inhaler depends on your symptoms, lung function, flare-up history, and how well you can use a specific device. Many people start with a long-acting bronchodilator, while others may need combination or triple therapy over time.
Is it bad to use a rescue inhaler every day?
Using a rescue inhaler daily usually means your COPD isn’t well controlled. It’s a sign to talk to your doctor about adjusting your maintenance inhaler rather than increasing rescue use.
Do steroid inhalers weaken the immune system?
Inhaled steroids act mainly in the lungs and are much safer than oral steroids. However, in some people they can increase the risk of pneumonia, which is why doctors prescribe them carefully and review their use regularly.
When do doctors recommend triple therapy inhalers?
Triple therapy (LABA + LAMA + ICS) is usually considered for people with persistent symptoms or frequent flare-ups despite dual therapy. It’s not a first-step treatment for most patients.
Can I switch inhalers if mine is hard to use?
Yes. If coordination, hand strength, or breathlessness makes an inhaler difficult to use, ask your doctor about a different device. Better technique often improves symptoms without changing medication.
References:
https://www.ncbi.nlm.nih.gov/books/NBK560073/
https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/treatment/
https://pmc.ncbi.nlm.nih.gov/articles/PMC3812880/
https://www.lung.org/blog/affordable-inhalers
https://my.clevelandclinic.org/health/treatments/17575-bronchodilator
https://publications.ersnet.org/content/erjor/5/1/00185-2018
https://www.copd.com/copd-treatment/daily-copd-maintenance-therapy/
https://www.mdpi.com/2227-9059/12/2/372
https://www.aaaai.org/tools-for-the-public/drug-guide/inhaled-corticosteroidshttps://goldcopd.org/wp-content/uploads/2024/11/GOLD-2025-Report-v1.0-15Nov2024_WMV.pdf



.avif)

.avif)


