Stage 2 COPD (Moderate): Symptoms, Treatment, Life Expectancy
This guide will walk you through what COPD stage 2 means for you, from understanding the GOLD stage 2 COPD criteria to outlining a modern stage 2 COPD treatment plan. The goal is to empower you with knowledge, so you can move forward with confidence and a clear action plan.

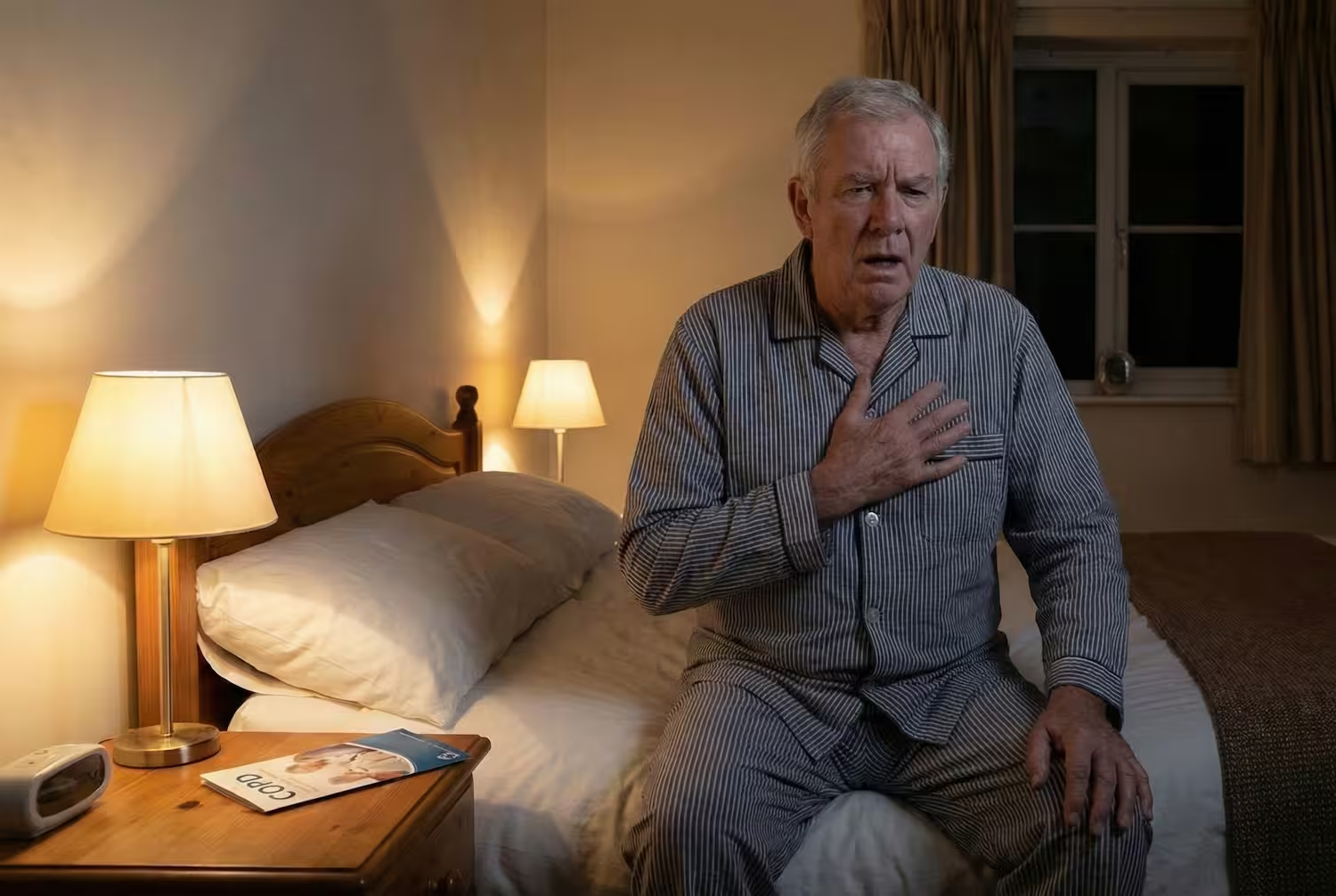
If you've been recently diagnosed with Stage 2 COPD, often called moderate COPD, you're likely experiencing symptoms that are harder to ignore. Perhaps you get short of breath walking on level ground, or a persistent cough has become a daily reality. It's common at this point to have questions like, "How bad is stage 2 COPD?" or "What is the life expectancy with stage 2 COPD?"
What Is COPD Stage II?
This stage is defined by a post-bronchodilator FEV₁ between 50% and 79% of the predicted value (based on GOLD 2025 guidelines).
In simpler words: your lungs still work, but airflow is reduced enough that you start feeling the difference.
Stage 2 is often a turning point. It’s the stage where doctors usually begin regular, long-acting inhalers, encourage pulmonary rehab, and help you create a long-term plan to prevent flare-ups and protect lung function. And with the right treatment and daily habits, many people stay stable in Stage 2 for years, sometimes even decades.
Symptoms of Stage 2 COPD
In Stage 2 COPD, symptoms become more noticeable and start affecting your daily routine.
You may still be able to do everything you used to, it just takes a little more effort, and you may need to slow down, take breaks, or adjust how you move through the day.
Primary Symptoms
The most common symptoms you're likely experiencing include:
Shortness of Breath (Dyspnea):
This is no longer just happening during heavy exertion. In moderate COPD, you may feel winded during routine activities like walking on level ground, carrying groceries, or even getting dressed. This is a key indicator of how bad stage 2 COPD has become.
Persistent Cough & Mucus:
A chronic, often productive cough is a hallmark. You might find yourself clearing your throat frequently, especially in the mornings.
Wheezing and Chest Tightness:
A whistling sound when you breathe or a feeling of pressure in your chest can occur as airflow becomes more obstructed.
Other Potential Symptoms
It's also important to know that COPD can have broader effects. While not everyone experiences them, some people report:
COPD and Nausea:
This can sometimes occur during severe coughing fits or as a side effect of increased mucus drainage.
COPD and Runny Nose:
Chronic respiratory conditions can sometimes be associated with post-nasal drip or non-allergic rhinitis.
COPD Foot Swelling:
Also known as edema, this can be a sign of cor pulmonale, a condition where COPD and heart failure are linked due to low oxygen levels, straining the right side of the heart. This symptom should always be reported to your doctor immediately.
During an examination, your doctor will listen for characteristic lung sounds in COPD, such as wheezing or diminished breath sounds, which confirm the airflow limitation.
Recognizing this full spectrum of symptoms is not meant to cause worry, but to empower you. Tracking these signs helps you and your doctor better evaluate your COPD stage 2 prognosis and adjust your treatment plan for optimal control.
How Moderate COPD Is Diagnosed
Diagnosis of COPD stage isn’t based on symptoms alone. It relies on spirometry, which measures how well your lungs move air in and out.
Stage 2 COPD is diagnosed when:
- FEV₁ is between 50% and 79% of the predicted value
- FEV₁/FVC is below 0.70 after using a bronchodilator
To understand how symptoms affect your life, doctors also use:
- CAT (COPD Assessment Test) - scores daily symptoms
- mMRC Dyspnea Scale - measures breathlessness during activity
You don’t need spirometry every month, but you do need consistent monitoring so your care plan stays on track. Doctors typically recommend Spirometry every 6–12 months.
Treatment & Medications at Level 2
Level 2 is often the point where treatment becomes more structured. This is also when doctors help you shift from relief-only treatments to a daily management plan designed to keep you stable long-term.
When to Start Daily Long-Acting Inhalers (LABA / LAMA)
In Stage 2, most patients begin maintenance inhalers, which help keep airways open throughout the day.
Your doctor may prescribe:
- LABA (Long-Acting Beta Agonist): relaxes the airway muscle
- LAMA (Long-Acting Muscarinic Antagonist): reduces airway tightening
- LABA + LAMA combination: if symptoms occur often or limit activity
These inhalers are taken once or twice daily, not just when symptoms appear.
When LABA + ICS May Be Considered
ICS = Inhaled Corticosteroids.
Doctors don’t automatically give steroids to all Stage 2 patients.
They’re used only if you:
- have two or more flare-ups per year,
- have been hospitalized for a severe exacerbation, or
- have elevated eosinophils (≥300 cells/μL), which suggests inflammation responds to steroids.
This combination helps prevent flare-ups, but since ICS can increase infection risk, doctors prescribe it carefully.
Role of Short-Acting Rescue Inhalers
You’ll still keep a rescue inhaler (like albuterol) on hand.
You are advised by your doctor to use it when:
- symptoms suddenly worsen,
- you’re doing physical activity, or
- you feel tightness or wheezing.
But it should not be your main treatment at Stage 2.
Pulmonary Rehabilitation (This Is the Stage to Start)
Pulmonary rehab is one of the most effective treatments for Stage 2 COPD, and many patients wish they started earlier.
These programs help you:
- improve breathing efficiency
- build endurance
- reduce breathlessness during activity
- strengthen respiratory muscles
- lower the risk of flare-ups
And you can do it from home with virtual options like CardaHealth, which increases consistency.
Lifestyle & Daily Habits
Medications work best when paired with simple daily habits:
- Quit smoking completely (the #1 way to protect remaining lung function)
- Stay active with daily walking or light exercise
- Eat high-protein, high-nutrient meals
- Avoid triggers like dust, chemical fumes, or cold air
Get vaccinated (flu, COVID, pneumococcal)
These habits directly affect how stable you’ll stay over the next few years.
Preventing and Managing Exacerbations or Flare-Ups
Exacerbations are also called flare-ups; these are sudden episodes when your breathing worsens quickly.
People with Stage 2 COPD are at higher risk of flare-ups than those in Stage 1, but most flare-ups can be prevented or controlled early if you know what to look for and what to do next.
Early Signs of Flare-ups to Notice
- Breathing becomes harder than usual
- Your regular inhaler doesn’t relieve symptoms
- Increased coughing or new wheezing
- Mucus becomes thicker or darker
- Chest tightness or discomfort
- Lower oxygen readings (if you use a pulse oximeter)
- Fever, chills, or flu-like symptoms
Recognizing these early signs is one of the most effective ways to prevent worsening.
Home Management Steps (What to Do First)
If a flare-up starts:
- Use your rescue inhaler exactly as your doctor prescribed.
- Practice pursed-lip breathing to regain control of your breath.
- Stay hydrated — warm fluids help loosen mucus.
- Avoid lying flat; sit upright or lean slightly forward.
Call Your Doctor if
- Symptoms worsen over 24–48 hours
- You need your rescue inhaler more often
- You feel unusually tired or dizzy
- You’re coughing up blood
- Your mucus changes color (green, brown, rusty)
Go to the ER immediately if:
- You’re struggling to breathe even at rest
- Your lips or fingertips look pale, gray, or blue
- You cannot speak in full sentences
- Your oxygen levels drop significantly (if monitored)
Quick action can protect your lungs from long-term damage.
Prognosis and Life Expectancy
It is one of the most common and understandable questions after a diagnosis: "What is the life expectancy with stage 2 COPD?" or "How long can you live with stage 2 COPD?" It's important to understand that a COPD stage 2 prognosis is not a predetermined expiration date. Instead, it's a projection that is actively and powerfully shaped by the choices you make and the treatments you follow.
So, how long does stage 2 COPD last? The disease itself is chronic and lifelong. However, the progression and its impact on your lifespan are highly variable. There is no one-size-fits-all life expectancy because many individual factors influence outcomes.
Your personal outlook depends heavily on smoking habits, treatment, and frequency of exacerbations. Each serious exacerbation can cause a permanent drop in lung function.
The question "is copd a death sentence?" can be answered with a resounding no. While it is a serious illness, it is also a manageable one. Many people live for decades with Stage 2 COPD by managing their condition proactively.
How to prevent Stage 2 from becoming Stage 3?
- Using maintenance inhalers daily
- Avoiding triggers (smoke, fumes, cold air)
- Staying active with regular exercise
- Getting vaccines (flu, COVID, pneumonia)
- Joining pulmonary rehab
- Treating flare-ups early
These habits significantly reduce the risk of rapid progression.
Stage 2 COPD and Disability
Another practical concern is, "does moderate copd qualify for disability?" The answer is, it can. Stage 2 COPD disability claims are evaluated based on how significantly your symptoms impair your ability to work. Medical documentation, including spirometry results and records of your symptoms and treatment, is essential for a successful claim.
Work, Travel & Lifestyle: Practical Tips
Stage 2 COPD doesn’t mean you have to slow down your life — it just means you need to plan a little smarter.
Most people at this stage continue working, traveling, and staying active with a few simple adjustments.
1. Work & Daily Routine
- Pace your tasks; break bigger tasks into smaller steps.
- Take short breathing breaks every 1–2 hours.
- Avoid heavy lifting or change how you carry weight (split loads, use carts).
- Check workplace air quality if exposed to dust, fumes, or chemicals.
- Keep your rescue inhaler nearby during long shifts or physical work.
- Plan walks or errands during the cooler parts of the day.
- Warm-up your chest muscles with gentle stretches before activity.
2. Traveling tips With COPD
- Carry your inhalers and medications in your hand luggage when flying.
- Move around during long flights to avoid stiffness and breathlessness.
- Check the weather and air quality at your destination: humidity, cold, and pollution can affect symptoms.
- If flying longer distances, ask your doctor whether you need an oxygen test before the trip.
4. Home Environment Adjustments
- Keep indoor air clean with good ventilation or a purifier.
- Avoid scented candles, strong cleaning chemicals, and aerosol sprays.
- Use a humidifier if your home is very dry (dry air can trigger coughing).
- Keep bedding dust-free. Wash sheets weekly in warm water
FAQs
1. Can Stage 2 COPD be reversed?
No. COPD at any stage cannot be fully reversed. But Stage 2 can remain stable for years for most patients with the right treatment, daily inhalers, and rehab. Many people maintain good activity levels without progressing quickly.
2. How long can I stay in Stage 2 COPD?
It varies. Some people stay in Stage 2 for many years, especially if they stop smoking and stay consistent with treatment. Progression is usually slower when flare-ups are prevented.
3. Do I need daily inhalers in Stage 2?
Yes, most patients do. Doctors usually prescribe long-acting bronchodilators (LABA or LAMA) at this stage because symptoms are more frequent and airways need steady support.
4. Will I need oxygen therapy at Stage 2?
Usually not. Most people in Stage 2 have normal or slightly lower oxygen levels at rest. Oxygen therapy is usually considered in later stages or during severe flare-ups.
5. Can I work with Stage 2 COPD?
Yes. Most people continue working full-time with small adjustments, such as pacing tasks, avoiding fumes or smoke, and keeping a rescue inhaler nearby.
6. Is Stage 2 COPD considered serious?
Stage 2 is moderate, not severe, but it’s still an important stage. With good management at this stage, people can stay active and prevent complications.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of COPD – 2025 Report.
- https://my.clevelandclinic.org/health/diagnostics/17833-spirometry
- National Heart, Lung, and Blood Institute (NHLBI). COPD – Diagnosis and Treatment.
- Mayo Clinic. Chronic obstructive pulmonary disease (COPD) – Treatment.
- Cleveland Clinic Journal of Medicine. Advances in COPD management and emerging therapies, 2024.





.avif)


