How to Increase Oxygen Levels: Safe Steps You Can Take at Home

When your oxygen levels drop or breathing suddenly feels harder, it can be scary. Maybe your chest feels tight. Maybe you looked at your pulse oximeter and saw a number lower than usual. Maybe you’re just worried because something feels “off.”
Take a slow breath with me.
Here are simple, safe ways you can use at home to help your body get the oxygen it needs. Let’s walk through what you can do, right now.
What Is a Normal Oxygen Level?
Your oxygen level is usually measured with a pulse oximeter, a small clip that goes on your finger and shows a number called SpO₂.
Here’s what those numbers generally mean:
If your oxygen is 88% or lower, especially with shortness of breath, get medical help right away. This condition is known as Hypoxemia.
What if I have COPD or another long-term lung condition?
Because your lungs have damage or blocked passages, the “normal” oxygen targets tend to be lower than for healthy people.
Some people with COPD, pulmonary fibrosis, or heart failure may have a different “normal” that their doctors set. Sometimes even 88–92% is acceptable for them.
So always follow your doctor’s targets if they give you a specific range.
Gains in oxygen above that range, especially when using supplemental oxygen, can also do more harm than good (by increasing carbon dioxide levels).
Also read: How to manage COPD at home?
What to Do Right Now if Your Oxygen Looks Low
If your pulse oximeter shows a lower number than usual, you don’t have to panic. These are safe, immediate methods you can try at home that might help raise your oxygen saturation and ease breathing, or at least help you assess what to do next.
1. Stay Calm & Check Carefully
- Sit or lie down comfortably. Anxiety can itself lower oxygen levels.
- Wait a minute, allow your breathing to settle.
- Make sure your finger (or toe) is warm and relaxed, and free of nail polish (cold or constricted fingers can give inaccurate readings).
- If your SpO₂ is below what’s usual for you (or below ~90 %), prepare to try a few supportive steps, but don’t assume it’s permanent.
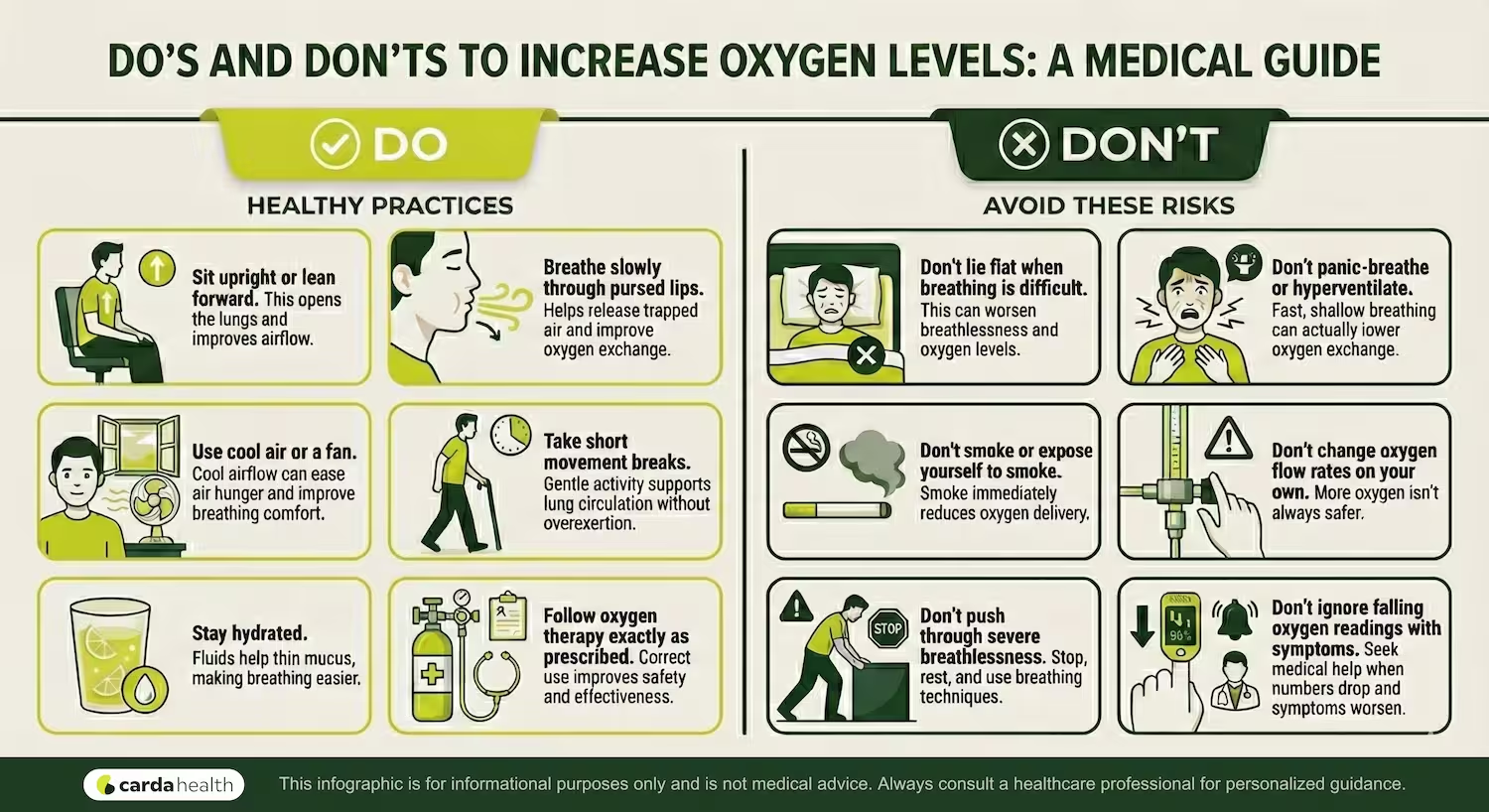
2. Quick Checks: If You Use Supplemental Oxygen
If you already use prescribed oxygen (via nasal cannula, concentrator, or tank):
Check that your oxygen source is actually working. (Empty tank? Power cut? Disconnected tube?) even simple failures cause drops. This is a common first check.
Verify flow settings: flow must match what your doctor prescribed. Don’t increase flow on your own. Over-oxygenation can be harmful for people with COPD or chronic lung disease.
3. Quick Breathing & Positioning Tricks (Try Right Now)
These are gentle, no-equipment moves that can help air get into your lungs more easily:
Pursed-lip breathing: Breathe in slowly through your nose, then exhale gently through pursed lips (like blowing out a candle). Helps release trapped air and slow breathing down.
Sit up or lean slightly forward: Resting your arms or elbows on your thighs or on a table helps your lungs open more fully than lying flat.
Turn on cool air / fan toward face: Cooler air can make breathing feel easier and may help lungs draw in oxygen better.
Stay seated, avoid rushing or exertion: Don’t try to stand or walk immediately if you feel light-headed or very breathless.
If after a few minutes you feel a bit better, breathing slows, tightness eases, check your SpO₂ again. If it improves, stay where you are and rest.
If nothing helps or things get worse, call your doctor or emergency services, immediately.
How to Sleep for Better Oxygenation
Here are practical sleep-time adjustments that often help breathing, especially if you have chronic lung disease, feeling breathlessness at night is highly common.
- Sleep with your head and chest raised
- Consider side-sleeping or semi-upright sleeping
- Keep the air clean and easy to breathe
- Avoid heavy meals, caffeine, or alcohol before sleep
- Use breathing techniques if you wake up breathless
Nutrition For High Oxygen Levels
What you eat, and how, matters a lot for your oxygen level. For lungs to work, your body needs energy, strong muscles, and minimal inflammation. Poor nutrition (or malnutrition) weakens respiratory muscles. In chronic lung disease, underweight or muscle loss often leads to worse breathing and lower oxygen levels.
Studies show that a healthy, balanced diet, rich in antioxidants, fiber, protein and healthy fats is linked with better lung function and may slow the decline of lung capacity over time.
So while food isn’t a medicine, it supports your lungs and body in a way that makes breathing easier and oxygen use more efficient.
Protein
Prioritize protein daily. Eggs, fish, poultry, beans, yogurt, they all help keep your breathing muscles strong.
Fats
Include healthy fats in your diet. Olive oil, nuts, seeds, fatty fish. These help with energy density and support body function with less strain on digestion.
Carbs & Fiber
Choose complex carbs + fiber. Whole grains, fruits, vegetables help keep inflammation down, and several curated studies link higher fiber intake with better lung function.
Hydration
Stay hydrated. Water (or non-caffeinated, non-sugary drinks) helps keep mucus thin, easier to clear, easier to breathe.
And overall, make sure that you eat small, frequent meals rather than large heavy meals, which can cause discomfort or bloating and make breathing harder. Good nutrition won’t immediately raise your oxygen saturation. But over weeks and months, it helps your body stay stronger, lungs clearer, and breathing muscles more capable, which improves your ability to maintain healthier oxygen levels.
If You Have COPD or a Chronic Lung or Heart Condition
If you’re living with COPD, pulmonary fibrosis, or another long-term condition, your body may already be working harder every day just to breathe. Your oxygen levels might not look like someone else’s.
Some people with chronic lung disease aim for 88–92% SpO₂, as guided by their care team.
So if your doctor gave you a specific target, that’s your number to watch, not the random charts online.
Oxygen Therapy Can Help
If your levels stay low even at rest or while sleeping, oxygen therapy may be recommended to take strain off your heart, and help you stay active. It prevents complications from chronic low oxygen.
If you already use oxygen, DO NOT change your flow rate without your doctor’s instructions.
Can Pulmonary Rehab Help You?
Guided exercise in pulmonary rehab programs build stronger breathing muscles, better endurance, so you lead to fewer flare-ups.
Carda offers a virtual pulmonary rehab program you can do at home, so you stay supported without unnecessary hospital visits.
When to Call a Doctor
Low oxygen can turn serious quickly. Knowing when to ask for help keeps you safe.
Call Your Doctor Soon If
Your oxygen level is:
- Less than your normal and not improving with breathing techniques
- Dropping more often than usual
- Accompanied by thicker mucus or more coughing
- Paired with new fatigue or confusion
These are signs your lungs need more support.
Get Emergency Help If
- SpO₂ stays below 88%, especially at rest
- Your lips, tongue, or fingertips turn blue or gray
- You feel very sleepy, confused, or dizzy
If you’re not sure whether to wait: don’t wait.
Call emergency services immediately.
Unsafe “Fixes” to Avoid (Myths)
When you’re struggling to breathe, it’s tempting to try anything that promises quick relief. But some common internet advice is not just unhelpful, it can be dangerous.
❌ Myth 1: “Just turn up your oxygen flow, more oxygen is better.”
Not true especially for COPD or chronic respiratory disease.
Higher oxygen flow without medical supervision can cause carbon dioxide retention, confusion, and even respiratory emergencies.
❌ Myth 2: Essential oils, incense, or steam “open the lungs.”
These smells and vapors can irritate airways, trigger coughing, worsen asthma/COPD or reduce airflow.
❌ Myth 3: “Just push yourself to breathe harder, your lungs will get stronger.”
Overexertion when oxygen is low can drop SpO₂ even further, and cause panic or dizziness.
❌ Myth 4: “Oxygen is all you need, no meds necessary.”
Conditions like COPD involve airway inflammation + mucus + trapped air. Oxygen alone does not fix those problems.
❌ Myth 5: “If you normally stay very still and avoid activity, you’ll save oxygen.”
Regular gentle activity, and exercises support oxygen levels.
Read: Pulmonary Rehab Exercises At Home
Conclusion
Low oxygen can feel scary, especially when it comes on suddenly. But now you have a simple plan:
- You know what the numbers mean
- You know what you can do right away
- You know what habits support better oxygen
- And you know when it’s important to call for help
And if you’re living with COPD or another chronic lung condition, having the right guidance can make breathing feel easier and safer at home. That’s exactly why Carda exists — to support you every day at home.
Talk to a CardaHealth specialist today and take the next step for your lungs.
FAQs
What is dangerously low oxygen?
For most people, below 92% is a sign you should call your doctor. Below 88% at rest may need urgent medical care. And if you have COPD or heart/lung disease, your doctor may give you a different target.
Can anxiety lower my oxygen level?
Anxiety usually doesn’t change oxygen directly, but it can make you breathe fast and shallow, which can lead to lower readings. Slow breathing often helps both the anxiety and the oxygen number.
How quickly should my oxygen improve after breathing exercises?
Many people see improvement within a few minutes if breathing exercises or position changes are going to help. If your levels don’t get better, call for medical advice.
Should I buy a home oxygen machine?
No, not without a prescription. Using oxygen incorrectly can be dangerous. Ask your doctor first if oxygen therapy is right for you.
Does drinking water help oxygen levels?
Yes! Staying hydrated helps keep mucus thin so air can move more easily through the lungs, especially in COPD.
References
https://my.clevelandclinic.org/health/diseases/17727-hypoxemia
https://www.physio-pedia.com/Pulse_Oximeter
https://pubmed.ncbi.nlm.nih.gov/33243839/
https://my.clevelandclinic.org/health/diagnostics/22447-blood-oxygen-level
https://www.mayoclinic.org/symptoms/hypoxemia/basics/definition/sym-20050930





.avif)


