Stage 3 COPD: Symptoms, Treatment & Life Expectancy
Chronic Obstructive Pulmonary Disease (COPD) is a long-term lung condition that makes it harder to breathe because the airways become narrow and inflamed over time.
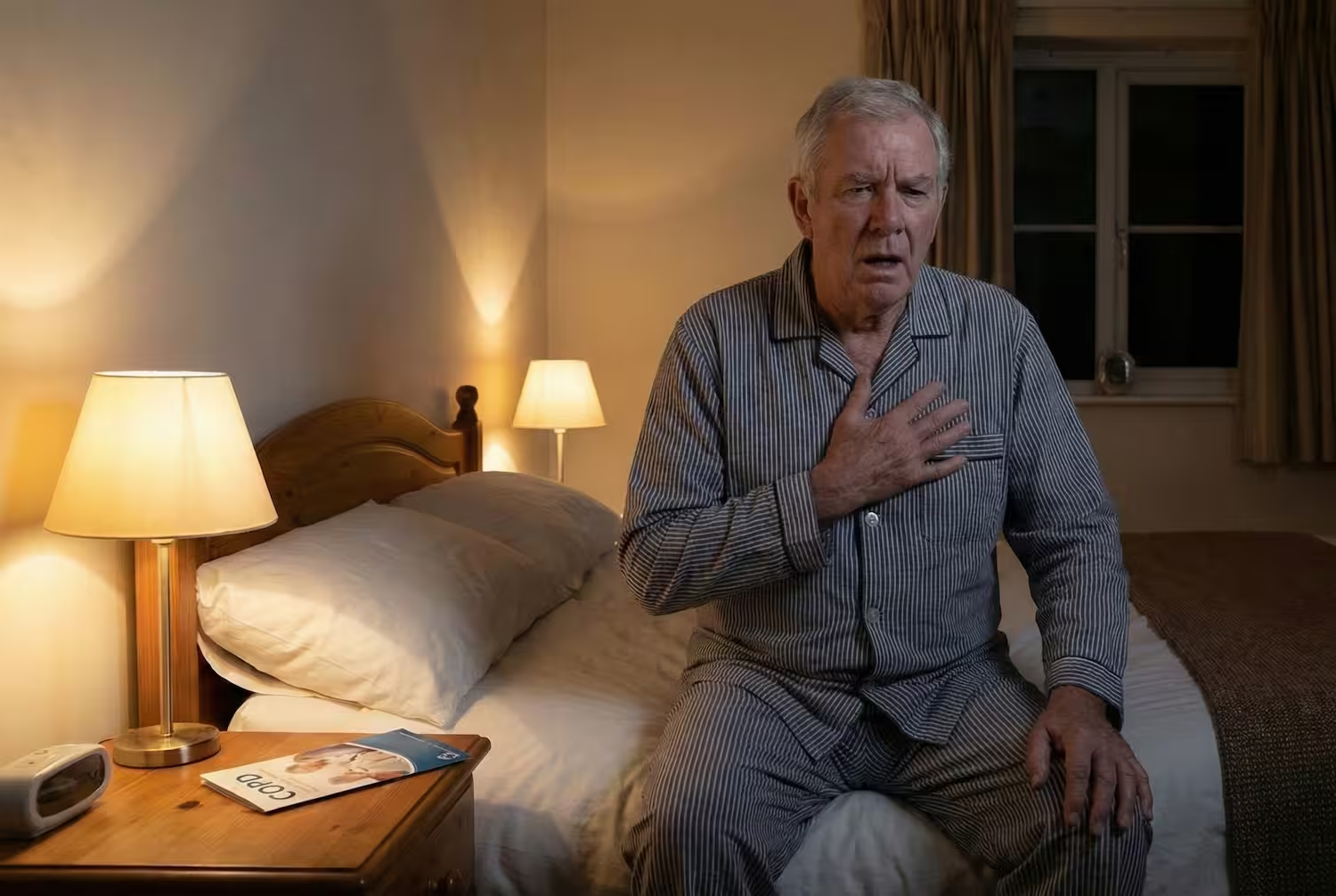
Stage 3 COPD means your lungs have developed a severe level of airflow limitation. At this stage, your lungs are working harder than before, and simple things like walking up stairs or carrying groceries might feel more tiring. But understanding what’s happening in your body can make things a lot less scary.

If you have recently been told about your COPD Stage Three, you might be feeling worried or confused - and that’s completely normal. But it doesn’t mean life stops here - it means your lungs need extra care, consistency, and the right treatment plan to keep symptoms under control.
In this guide, we’ll walk through:
- What Stage 3 COPD really means in medical terms
- The symptoms you can expect and how they differ from earlier stages
- The treatments that help you breathe easier and live more comfortably
- And how lifestyle choices and rehabilitation can make a real difference.
What Is GOLD Stage 3 COPD?
Doctors use a system called the GOLD staging (Global Initiative for Chronic Obstructive Lung Disease) to classify the severity of COPD. It’s based mainly on a breathing test called spirometry, which measures how much air you can exhale in one second - known as your FEV₁ (Forced Expiratory Volume in 1 second).
In Stage 3 COPD, the FEV₁ value falls between 30% and 49% of what’s expected for your age, sex, and height after using a bronchodilator. That means your lungs can push out less than half the normal amount of air in one second — which explains why breathing can feel so difficult.
Common Symptoms
At stage 3, symptoms become much more noticeable and often affect daily life. Here’s what you may experience:
- Shortness of breath (even during light activity or rest)
- Chronic cough with mucus production
- Wheezing or chest tightness
- Frequent infections or flare-ups (bronchitis, pneumonia)
- Fatigue and low energy
- Unintentional weight or muscle loss
- Swelling in ankles or legs (a sign of heart strain)
In earlier stages, these symptoms might come and go.
By Stage 3, they often become part of daily life - but still manageable with treatment.
How Doctors Diagnose Stage 3 COPD
The main test used is spirometry - a simple breathing test where you blow air into a device called a spirometer. This measures your FEV₁ (how much air you can exhale in one second) and your FVC (total amount of air you can blow out after a deep breath).
If your FEV₁ is between 30% and 49% of the predicted value, it confirms Stage 3 (severe) COPD, according to the GOLD 2025 guidelines.
Doctors may also order other tests to get a full picture of your health, including: Pulse oximetry, Arterial blood gas (ABG), Chest X-ray or CT scan, Six-minute walk test, etc.
Once Stage 3 COPD is confirmed, your doctor may recommend regular follow-ups - usually every 3–6 months.
WHY? COPD is a progressive condition, but the pace can vary. Some people stay stable for years with proper care. Routine check-ups ensure that your treatment, exercise plan, and oxygen support stay aligned with your current lung health.
Treatment Options
There isn’t a single “cure” for COPD, but there is a clear path to slowing its progression and improving how you feel day-to-day. With the right combination of medication, therapy, and lifestyle support, many people manage their symptoms, stay active, and enjoy meaningful quality of life for years.
1. Medication
Most treatment plans include inhaled medicines that relax and open your airways.
Long-acting bronchodilators (LABA or LAMA): They relax airway muscles for up to 12–24 hours, making breathing easier throughout the day.
Examples: tiotropium, salmeterol, formoterol.
Combination inhalers (LABA + ICS): Contains a small dose of inhaled corticosteroid (ICS) to reduce airway inflammation and lower the risk of flare-ups.
Short-acting bronchodilators: Used as “rescue inhalers” for sudden breathlessness. Always keep one close.
Oral medications: In certain cases, drugs like roflumilast (to reduce inflammation) or theophylline (to relax muscles in the airways) may be added if symptoms remain severe.
DO NOT TAKE ANY MEDICINE WITHOUT YOUR DOCTOR’S PERMISSION.
2. Pulmonary Rehabilitation Programs
Among all non-drug treatments, pulmonary rehabilitation has the strongest evidence for improving life quality in Stage 3 COPD.
Research shows rehab can:
- Improve breathing efficiency and endurance.
- Reduce flare-ups and hospital visits.
- Boost energy and confidence in daily life.
Carda Health’s virtual pulmonary rehab brings this care right to your home - guided by licensed clinicians who help you exercise safely, track progress, and regain control over your breathing without long clinic commutes.
3. Oxygen Therapy
If blood oxygen levels fall below safe limits, your doctor may recommend supplemental oxygen.
It helps relieve breathlessness, protects vital organs, and can even extend life expectancy when used as prescribed.
4. Preventing Flare-Ups (Exacerbations)
Flare-ups are sudden episodes where symptoms sharply worsen. They can speed up lung damage, so prevention is key.
- Stay up to date on vaccines
- Avoid smoke, fumes, and pollution.
- Wash hands more often
5. Lifestyle and Self-Care Changes
Small daily habits like quitting smoking completely, eating balanced and high-protein meals, practicing breathing techniques, and getting enough sleep can have a big impact.
6. New and Advanced Therapies
Medical research is ongoing.
Doctors are testing biologic medicines (like dupilumab) for COPD with specific inflammation patterns, and lung-volume-reduction surgery or endoscopic valves for select cases where damaged lung areas can be isolated.
While not suitable for everyone, these advances show how treatment for COPD continues to evolve.
Life Expectancy & Outlook
There’s no exact timeline for Stage 3 COPD - everyone’s journey is unique.
Doctors use tools like the BODE index (Body Mass, Obstruction, Dyspnea, and Exercise capacity) to estimate outcomes, factoring in lung function, weight, symptoms, and activity level.
On average, Stage 3 COPD can shorten life expectancy by around 5–6 years compared to people without COPD, but many live far longer when they stay consistent with care .
How To Improve Outlook:
- Take medications as prescribed
- Join a pulmonary rehab program
- Get vaccinated
- Eat well and stay active
Living Life with Stage 3 COPD
Living well with COPD means building basic habits that support your lungs and conserve energy.
Gentle activity keeps your lungs efficient. Light walking or resistance exercises help maintain strength, just pace yourself and rest when needed. Besides, build following habits:
✔️ Practice breathing exercises regularly
✔️ Prioritize protein, fresh produce, and hydration.
✔️ Eat smaller, frequent meals to avoid feeling breathless.
✔️ Sit while cooking or folding laundry.
✔️ Keep essentials within easy reach.
✔️ Avoid strong scents or cleaning fumes.
✔️ Rest in a slightly elevated position.
Seek Emergency Help If:
- You’re struggling to breathe even while resting.
- Your lips or fingertips turn blue or gray (sign of low oxygen).
- You can’t speak in full sentences without gasping.
Conclusion
Stage 3 COPD can feel overwhelming at first, but with the right care, support, and mindset, many people continue to live active and meaningful lives for years.
While you stay consistent with medication and nutrition, non-medical treatments like pulmonary rehab can also help you breathe easier, move better, and feel stronger every day.
Check out CardaHealth’s virtual pulmonary rehab, making expert care accessible from home.
FAQs
1. Can Stage 3 COPD be reversed?
No, but it can be controlled. Treatment focuses on slowing progression and improving comfort.
2. What’s the FEV₁ range for Stage 3 COPD?
Between 30% and 49% of predicted after bronchodilator use.
3. How long can someone live with Stage 3 COPD?
Many people live for years, even a decade, with proper treatment and rehab.
4. How can I slow down COPD progression?
Quit smoking, use inhalers correctly, wash your hands more often, attend pulmonary rehab, go for regular check-ups, and avoid infections.
5. How is Stage 3 different from Stage 4 COPD?
Stage 3 is severe but can be managed with proper treatment. Stage 4 is the most severe, often requiring continuous oxygen and more frequent hospital care.
Sources
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management, and Prevention of COPD – 2025 Report.
- National Heart, Lung, and Blood Institute (NHLBI). COPD – Diagnosis and Treatment.
- Mayo Clinic. Chronic obstructive pulmonary disease (COPD) – Treatment.
- Cleveland Clinic Journal of Medicine. Advances in COPD management and emerging therapies, 2024.
- Celli BR et al. The BODE Index in Chronic Obstructive Pulmonary Disease. N Engl J Med.
- Verywell Health. Stage 3 COPD: Symptoms, Treatment, and Life Expectancy, 2024 Update.





.avif)


