Heart failure is a serious medical condition that occurs when the heart muscle cannot pump enough blood to the rest of the body's tissues and organs. Sometimes, heart failure can worsen significantly and progress into decompensated heart failure.
What is this type of heart failure, and how does it compare to compensated heart failure? Carda is here to discuss decompensated heart failure today, including its symptoms, causes, and treatment options. Read on to support your cardiovascular health.
What Is Decompensated Heart Failure?
Decompensated heart failure occurs when the symptoms of heart failure require a person to seek immediate medical care. "Decompensated" means that the heart was previously functioning but has deteriorated such that it can no longer compensate for its malfunctions.
Heart failure can be acute or chronic. With acute decompensated heart failure, a person has no prior signs or symptoms before developing this life-threatening disease onset. However, with chronic heart failure, a person slowly develops progressive heart failure with evident signs and symptoms.
What Is Compensated Heart Failure?
In contrast, when a person has heart failure but does not experience any symptoms yet, their heart failure is called compensated heart failure.
What Are the Symptoms of Decompensated Heart Failure?
With decompensated heart failure, the heart cannot make up for its inability to pump enough blood to the rest of the body. The circulation dysfunction can cause a buildup of pressure and fluid retention in the circulatory system.
The pressure buildup and fluid retention may cause swelling, or edema, in the legs, feet, and abdomen, as well as pulmonary congestion. In addition, decompensated heart failure can cause symptoms such as weight changes, wheezing, coughing, an irregular heartbeat, or shortness of breath.
Weight Changes
Weight gain in a short amount of time may indicate that heart failure is worsening. If your weight increases more than several pounds within 24 hours or by more than five pounds in one week, you should check in with your healthcare provider regarding your condition.
Wheezing and Coughing
Poor circulation due to inadequate blood flow can cause fluid and pressure buildup in the circulatory system. This can cause fluid retention in other areas, including the lungs.
Wheezing and coughing, as well as chest discomfort and pain, are common response symptoms to this lung fluid buildup. When a person has decompensated heart failure, the wheezing and coughing are more likely to persist for long periods of time without going away.
Irregular Heartbeat
An irregular heartbeat, also called an arrhythmia, happens when your heart either beats too fast or too slow or skips a beat. The out-of-rhythm heartbeat can affect the heart's pumping mechanism, which means the amount of blood flow that goes to the rest of the body can decrease.
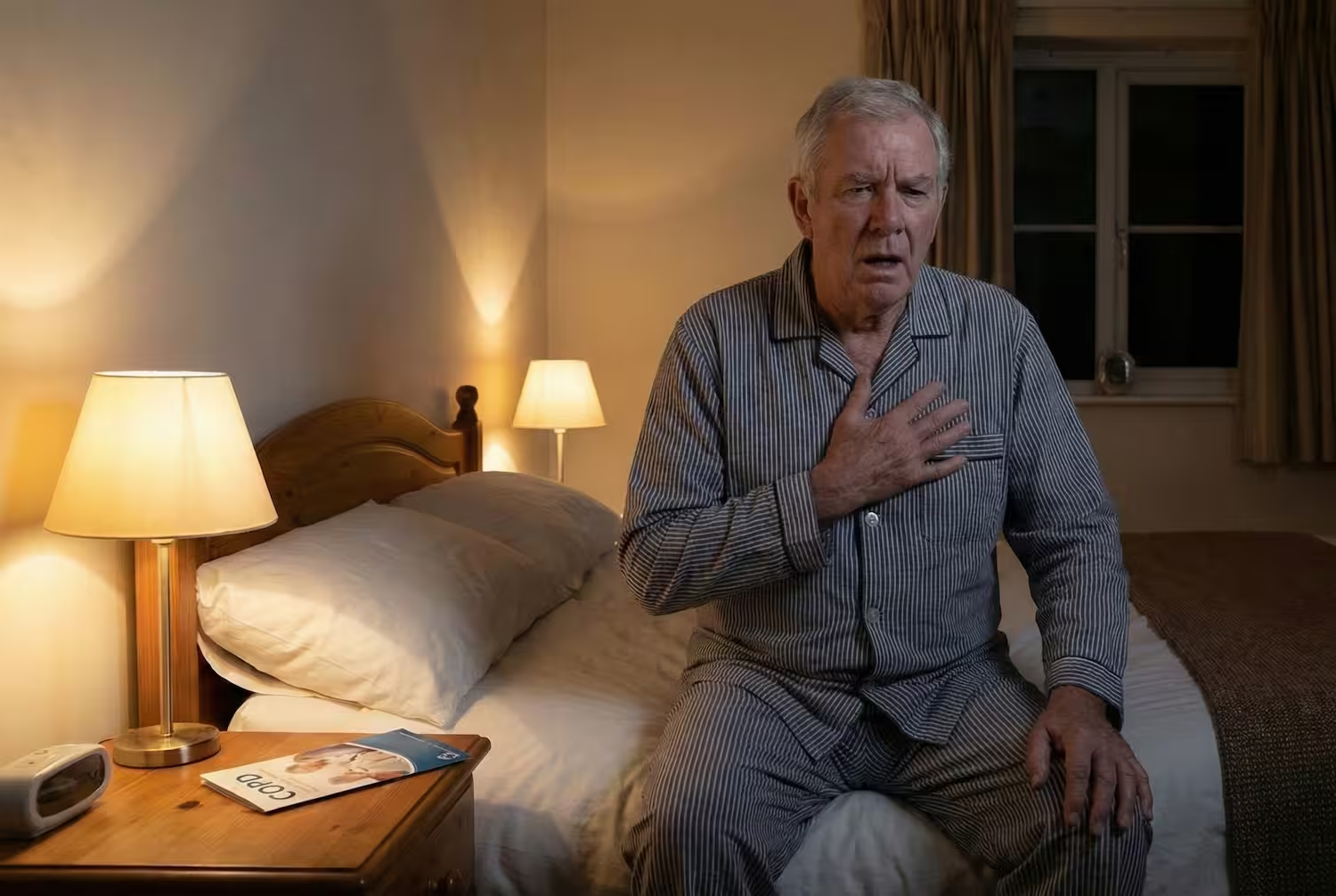
Shortness of Breath
Shortness of breath, also known as dyspnea, is one of the most recognizable and prevalent symptoms of decompensated congestive heart failure. A person with this heart disease may often experience shortness of breath with physical exertion but also can experience shortness of breath while lying down or staying stationary.
Dyspnea can often indicate the progression of heart failure — the more prevalent this symptom is, the more likely it is that this heart disease has worsened.
What Causes Decompensated Heart Failure?
The causes of decompensated heart failure include certain health conditions, dietary risk factors, and biological risk factors. Let's take a more in-depth look at each of these causes next.
Certain Health Conditions
If a compensated heart failure patient has pre-existing cardiac health conditions which worsen, they may develop decompensated heart failure. This can be true even if the patient is following their cardiac wellness plan.
Underlying heart-related conditions that can place a person at risk for decompensated heart failure include:
- Heart attack
- High blood pressure (hypertension)
- Heart inflammation (myocarditis)
- Cardiomyopathy
- Systolic or diastolic heart disease
- Heart valve disease
- Heart arrhythmia
Dietary Risk Factors
Certain dietary habits can increase a person's risk of developing decompensated heart failure. A diet high in salt or excess water consumption is a risk factor because heart failure often already leads to a fluid buildup in the body.
Consuming excess amounts of water only further contributes to fluid buildup. Additionally, salt attracts fluid, so if a person eats a high amount of sodium, this can also contribute to a large amount of fluid retention. Diets high in salt may also elevate blood pressure levels, which only further places someone at risk for heart failure to progress.
To help lower the amount of sodium you consume in your diet, try to limit the amount of processed or refined foods you eat. Always check labels for sodium content, and when you are cooking at home, substitute other spices like garlic, paprika, onion powder, or rosemary in place of salt.

Biological Risk Factors
A family history of heart disease, especially heart failure, places a person at an increased risk of developing heart failure that could turn into decompensated heart failure. Family members can pass on traits through genes.
Additionally, certain gene mutations can weaken or stiffen someone's heart tissue, making them more prone to developing heart failure.
How Is Decompensated Heart Failure Treated?
There are several different ways to treat decompensated heart failure. Each strategy involves aggressively addressing the underlying causes. Options for the management of heart failure can include medications, surgery, cardiac rehabilitation, or a combination of several or all of these different methods. Let’s explore each of them a little bit more in-depth below.
Medications
Medications such as diuretics can help to relieve the discomfort from some of the symptoms like fluid retention and swelling. Additionally, a cardiologist or healthcare provider might prescribe beta-blockers or ACE inhibitors and ARBs.
ACE inhibitors, or angiotensin-converting enzyme inhibitors, as well as ARBs (which are angiotensin receptor blockers), can help decrease high blood pressure. Beta-blockers can help alleviate pressure on the heart muscle.
Surgery
If there is an underlying cardiac-related condition that is causing decompensated heart failure, then a medical procedure or surgery to address the underlying cause is a treatment option. For example, if a patient has a leaky or defective heart valve, a heart valve surgery that replaces or fixes the malfunctioning valve may help address the decompensation.
Cardiology can also perform a heart transplant surgery to give a person a new and healthy functioning heart.
Cardiac Rehabilitation
Finally, a cardiac rehabilitation program can help a person develop stress management techniques to help lower blood pressure or target other underlying heart conditions that could be contributing to decompensated heart failure. Cardiac rehabilitation is an outpatient program that people can participate in once they get a referral from their healthcare provider.
In cardiac rehab, heart failure patients experience frequent provider healthcare guidance and education on cardiac health. They learn about heart-healthy diets, make plans to manage their stress to help increase their cardiac wellness, and engage in physiologist-guided exercise to help strengthen their heart muscle.
With virtual cardiac rehab through Carda, you can have the same provider throughout your rehab journey to be able to develop a strong working relationship that strives to achieve unique goals in your cardiovascular recovery process. Additionally, you get to choose when and where you do your rehab, and everything feels easy with the at-home vitals monitoring and cardiac care kit that Carda sends.
Signing up is easy — just fill out our simple form online and get a referral from your healthcare provider.
The Bottom Line
Decompensated heart failure is a life-threatening cardiac condition in which the symptoms of heart failure progress to medical emergency status. While a patient with heart failure may be able to manage their symptoms, decompensated heart failure greatly affects a person's quality of life and can result in organ failure without prompt treatment.
Underlying cardiac health conditions are a prevalent cause of decompensated heart failure, as they can damage the heart. There are also dietary and biological risk factors that can contribute to a decompensated heart failure diagnosis.
Fortunately, many treatment options can help a person manage their disease and have a good outlook that overcomes mortality rates. If you have decompensated heart failure, talk to your healthcare provider today about getting a referral for cardiac rehabilitation to reinforce your cardiovascular healing journey and improve your overall cardiac wellness.
Sources:
Managing Heart Failure Symptoms | American Heart Association (AHA)
Heart Failure - Causes and Risk Factors | NHLBI, NIH
Acute Heart Failure: Types, Symptoms, Causes and Treatment | Cleveland Clinic