If you or a loved one has congestive heart failure, the diagnosis can feel daunting. However, this disease has several stages, and not every stage is severe. Moreover, there are many different treatment options in the later stages of this disease that can help manage symptoms to slow disease progression.
Today, Carda is here to talk about congestive heart failure and what this diagnosis means. We will cover each of the stages in detail, including their hallmark symptoms as well as treatment options. Read on to support your cardiovascular health and wellness with Carda.
What Is Congestive Heart Failure?
Congestive heart failure (CHF) occurs when your heart muscle can no longer pump enough blood supply to the rest of your body. This causes blood buildup or backup in the heart and fluid retention in your lungs, feet, arms, and other parts of your body.
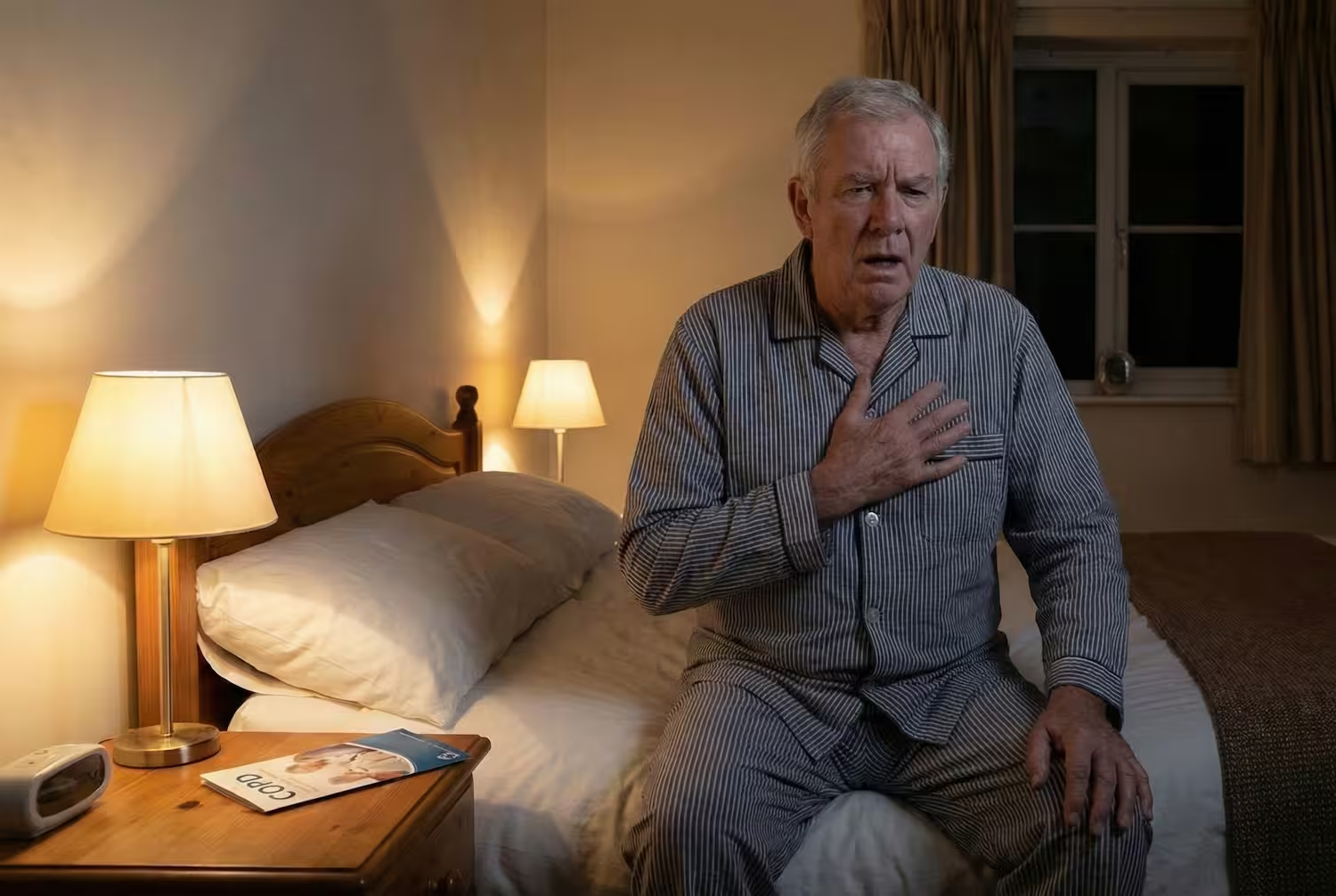
Common signs and symptoms of congestive heart failure include heart palpitations, tachycardia (rapid heartbeat), shortness of breath, difficulty breathing, fatigue, muscle weakness, a persistent cough, swelling in different body parts (legs, ankles, feet, or stomach), nausea, or chest pain.
Fluid buildup, or edema, is often a hallmark symptom of congestive heart failure. When a person experiences edema in their legs, coupled with shortness of breath, severe fatigue, heart palpitations, and chest discomfort, it is likely that they are experiencing congestive heart failure.
What Are the Main Causes of Congestive Heart Failure?
Medical conditions that affect the heart's function and structure are the main causes of heart failure. Narrowed or blocked coronary arteries, also known as coronary artery disease (CAD), is the leading cause of congestive heart failure. Your coronary arteries are the passageways that supply oxygen-rich blood to your heart and help your heart pump blood out to the rest of your body.
However, with certain risk factors such as high cholesterol levels, high blood pressure, an unhealthy lifestyle, repeated exposure to stress, obesity, and smoking, a coronary artery can develop a blockage that prevents adequate blood flow from getting to the heart.
In addition to CAD, there are other less common causes of congestive heart failure. These causes include infection, an autoimmune disease, a blunt trauma that affects the heart muscle, or certain medical treatments like chemotherapy or exposure to radiation therapy.
What Are the Main Stages of Congestive Heart Failure?
There are four main stages of congestive heart failure, ranging from an initial stage (stage A) to a final stage (stage D). Let's explore each of these stages below.
1. Stage A: Pre-Heart Failure
At this initial stage of congestive heart failure, the heart can still pump enough blood to the rest of the body. Rather, there are other chronic conditions that a person has that make them very susceptible to developing a more advanced version of congestive heart failure.
If a person has coronary artery disease, for example, their doctor will likely diagnose them with stage A congestive heart failure. High blood pressure (hypertension), diabetes, and metabolic syndrome are also risk factors that can place someone in stage A for CHF.
Because this first stage does not involve the heart failing to pump enough blood to the rest of the body yet, there are no symptoms of stage A congestive heart failure. However, there are associated symptoms from chronic diseases that closely align.
These symptoms can include shortness of breath, wheezing, or other difficulties breathing. They can also include chest discomfort or swelling in a person's hands, feet, or legs.
2. Stage B: Pre-Heart Failure
During stage B of congestive heart failure, the heart muscle does begin to experience a slightly diminished ability to pump blood. As a result, the left ventricle area of the heart may start to enlarge during this stage.
There are not often new symptoms that present at this stage of the condition other than the associated symptoms that present with another chronic condition.
3. Stage C: Heart Failure Diagnosis
Stage C involves more difficulties with the left ventricle of the heart, such that it is not only enlarged but also has trouble pumping blood. Its diminished ability to squeeze, or pump blood, out often leads people to experience more severe shortness of breath, fatigue, muscle weakness, and chest discomfort.
While stages A and B are technically "pre" heart failure, stage C involves an official heart failure diagnosis. People at this stage will often notice that day-to-day tasks are harder to accomplish due to difficulties in movement and shortness of breath with even simple activities.
4. Stage D: Advanced Symptoms
Stage D is the most severe phase of congestive heart failure, during which the heart's ability to pump blood drastically decreases.
Signs and symptoms at this stage can include:
- Trouble breathing
- Fatigue
- Muscle weakness
- Heart palpitations
- A chronic cough
- Nausea
- Unexplained weight gain
- Edema (swelling) in the legs, arms, hands, feet, and stomach area
At this most advanced stage, people may experience shortness of breath and fatigue while resting. Blood pressure drops significantly during stage D, and other organs can start to fail, which can cause kidney or liver disease.
What Might Treatment Entail for Each Stage of Congestive Heart Failure?
Treatment efforts vary depending on which stage of congestive heart failure you are dealing with. Here is a closer look at what treatment might entail for each stage.
Stage A Treatment
During stage A of congestive heart failure, the best treatment options are preventative measures to help slow or stop the disease's advancement. These preventative measures are usually lifestyle changes, such as eating a heart-healthy diet and staying physically active.
If you have risk factors for CHF, such as high blood pressure and high cholesterol levels, then your doctor may also focus on lowering these levels through medications. Smoking and drinking are additional risk factors, so if you engage in either of these activities, then part of the treatment during stage A includes quitting smoking or abstaining from drinking alcohol.
Stage B Treatment
Stage B builds off the treatment plan for stage A to add in more medication options. Medication options include an angiotensin-converting enzyme (ACE) inhibitor to help lower your blood pressure or a beta blocker to regulate your heart rate and also help lower your blood pressure.
If you have coronary artery disease, your doctor might start to develop a surgery plan for a procedure that relieves the artery blockage to alleviate blood flow and supply to the heart.
Stage C Treatment
Stage C will often include additional medications, such as SGLT2 inhibitors and Entresto (a blood pressure medication), which can decrease a patient's risk for hospitalization or death.
SGLT2, or sodium-glucose cotransporter-2, inhibitors are medication options that can help lower your blood sugar. Even if a person does not have diabetes, these inhibitors can help reduce a person's risk of a hospital stay or death during CHF. Additional medication choices that your primary care provider might offer you at this stage include Aldosterone antagonists, Ivabradine, or Digoxin.
A medical intervention, such as a biventricular pacemaker or an implantable cardiac defibrillator, may also be a treatment option that your doctor pursues at this stage.
A biventricular pacemaker helps your heart to pump blood more efficiently to the rest of your body. While it cannot treat CHF, it can help alleviate your symptoms to improve your quality of life at this stage. An implantable cardiac defibrillator (ICD) may also not treat or eliminate CHF, but it can help to enhance your quality of life. An ICD monitors and attempts to help correct heart arrhythmias, speeding up or slowing down the beat to bring it back down to a normal rhythm.
Stage D Treatment
At the most severe and advanced stage of CHF, you will likely need heart surgery or a heart transplant in order to survive. An additional support option to supplement a surgical procedure includes mechanical circulatory support to help blood circulate to the rest of your body and to keep your other organs functioning.
Moreover, your support team can continue offering you IV medications that support your heart muscle and help sustain its strength.

The Bottom Line
Congestive heart failure is a serious medical condition that affects the heart’s ability to function. With CHF, the heart muscle cannot properly pump enough blood supply to the rest of the body. Early to mid symptoms include shortness of breath, coughing, dizziness, chest discomfort, and swelling in the legs, feet, and ankles.
As the disease progresses, symptoms continue to worsen and can ultimately cause organ failures and severe difficulty in breathing and moving.
There are four stages to CHF, each one progressively worse than the last. While the first two stages are pre-heart failure stages and are easier to treat and prevent progression, once someone experiences stages C and D of the disease, it is much harder to treat.
Fortunately, there are many different ways to help manage the disease in its later stages. Joining a cardiac rehabilitation program like Carda’s is a great way to boost your mental outlook and experience support during your CHF journey.
Sources:
Congestive Heart Failure (CHF) Fact Sheets | Yale Medicine
Heart failure - Diagnosis and treatment | Mayo Clinic
Medications Used to Treat Heart Failure | AHA